Abstract
Since the publication of To Err Is Human: Building a Safer Health System in 1999, there has been much research conducted into the epidemiology, nature and causes of medication errors in children, from prescribing and supply to administration. It is reassuring to see growing evidence of improving medication safety in children; however, based on media reports, it can be seen that serious and fatal medication errors still occur. This critical opinion article examines the problem of medication errors in children and provides recommendations for research, training of healthcare professionals and a culture shift towards dealing with medication errors. There are three factors that we need to consider to unravel what is missing and why fatal medication errors still occur. (1) Who is involved and affected by the medication error? (2) What factors hinder staff and organisations from learning from mistakes? Does the fear of litigation and criminal charges deter healthcare professionals from voluntarily reporting medication errors? (3) What are the educational needs required to prevent medication errors? It is important to educate future healthcare professionals about medication errors and human factors to prevent these from happening. Further research is required to apply aviation’s ‘black box’ principles in healthcare to record and learn from near misses and errors to prevent future events. There is an urgent need for the black box investigations to be published and made public for the benefit of other organisations that may have similar potential risks for adverse events. International sharing of investigations and learning is also needed.
Similar content being viewed by others
References
Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academy Press; 2000.
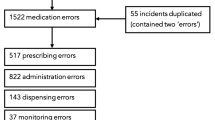
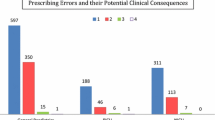
Ghaleb M, Barber N, Franklin B, et al. The incidence and nature of prescribing and medication administration errors in paediatric inpatients. Arch Dis Child. 2010;95:113–8.
Wong IC, Ghaleb MA, Franklin BD, et al. Incidence and nature of dosing errors in paediatric medications. A systematic review. Drug Saf. 2004;27:661–70.
Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;2001(281):2114–20.
Jani YH, Barber N, Wong ICK. Paediatric dosing errors before and after electronic prescribing. Qual Saf Health Care. 2010;19:337–40.
Terry DRP, Solanki GA, Sinclair AG, et al. Medicines reconciliation on admission—don’t forget the children. Br J Clin Pharm. 2009;1:22 (Abstract).
Huynh C, Tomlin S, Jani Y, et al. An evaluation of the epidemiology of medication discrepancies and clinical significance of medicines reconciliation in children admitted to hospital. Arch Dis Child. 2016;101:67–71.
Butler E, Bourke C. Medicine reconciliation on admission in a paediatric hospital setting. Arch Dis Child. 2013. doi:10.1136/archdischild-2013-303935b.4. (Abstract).
Huynh C, Wong I, Tomlin S, et al. An evaluation of paediatric medicines reconciliation at hospital discharge into the community. Int J Pharm Pract. 2016;24:196–202.
Alenezi S, Abramson J, Smith C, et al. Interventions made by UK pharmacists to minimise risk from paediatric prescribing errors. Arch Dis Child. 2016. doi:10.1136/archdischild-2016-311535.65. (Abstract).
Booth R, Sturgess E, Taberner-Stokes A, et al. Zero tolerance prescribing: a strategy to reduce prescribing errors on the paediatric intensive care unit. Intens Care Med. 2012;38:1858–67.
World Health Organization. Action on patient safety—high 5s. 2016. http://www.who.int/patientsafety/implementation/solutions/high5s/en/. Accessed 17 Dec 2016.
Morris S, Rivett C. The development of a quality improvement system to monitor, assess and feedback prescribing errors in paediatric intensive care. Arch Dis Child. 2016. doi:10.1136/archdischild-2016-311535.42. (abstract).
Alenezi S, Sammons H, Conroy S. Educational interventions to reduce paediatric prescribing errors. Arch Dis Child. 2015. doi:10.1136/archdischild-2015-308634.9. (abstract).
Telegraph newspaper. Baby died after GP surgery issued wrong prescription. 2010. http://www.telegraph.co.uk/news/uknews/7457772/Baby-died-after-GP-surgery-issued-wrong-prescription.html. Accessed 1 Aug 2016.
Daily Mail newspaper. Father commits suicide after being wrongly blamed by hate mob for death of baby daughter caused by GP error. 2010. http://www.dailymail.co.uk/news/article-1258410/Father-wrongly-blamed-hate-mob-death-daughter-caused-GP-error-committed-suicide.html. Accessed 1 Aug 2016.
Grissinger M. Too many abandon the “Second Victims” of medical errors. Pharm Ther. 2014;39(9):591–2.
National Transportation Safety Board. USA. Cockpit voice recorders (CVR) and flight data recorders (FDR). http://www.ntsb.gov/news/Pages/cvr_fdr.aspx. Accessed 16 Dec 2016.
Kapur N, Parand A, Soukup T, et al. Aviation and healthcare: a comparative review with implications for patient safety. J Roy Soc Med Open. 2015;7(1):2054270415616548.
Dekker S. The criminalization of human error in aviation and healthcare: a review. Saf Sci. 2011;49:121–7.
Former Locum handed suspended jail term for dispensing error. Pharm J. 2009. http://www.pharmaceutical-journal.com/news-and-analysis/former-locum-handed-suspended-jail-term-for-dispensing-error/10882780.article. Accessed 3 Feb 2017.
Elizabeth Lee case raises novel questions on interpretation of Medicines Act, judges say. Pharm J. 2010. http://www.pharmaceutical-journal.com/opinion/correspondence/elizabeth-lee-case-raises-novel-questions-on-interpretation-of-medicines-act-judges-say/11015210.article. Accessed 30 Oct 2016.
BBC News. ‘Overworked’ pharmacist ‘gave woman wrong pills’. 2016. http://www.bbc.co.uk/news/uk-northern-ireland-38223865. Accessed 17 Dec 2016.
Guardian Newspaper. Suspended sentence for optometrist who missed boy’s fatal condition. 2016. https://www.theguardian.com/uk-news/2016/aug/26/suspended-sentence-for-optometrist-who-missed-boys-fatal-condition. Accessed 30 Oct 2016.
Acute Care ISMP Medication Safety Alert! Eric Cropp weighs in on the error that sent him to prison. 2009. https://www.ismp.org/newsletters/acutecare/articles/20091203.asp. Accessed 30 Oct 2016.
Hartnell N, MacKinnon N, Sketris I, et al. Identifying, understanding and overcoming barriers to medication error reporting in hospitals: a focus group study. BMJ Saf Qual. 2012;21:361–8.
European Commission, Patient Safety and Quality of Care working group. Key findings and recommendations on Reporting and learning systems for patient safety incidents across Europe. 2014. http://ec.europa.eu/health//sites/health/files/patient_safety/docs/guidelines_psqcwg_reporting_learningsystems_en.pdf. Accessed 22 Dec 2016.
Nursing and Midwifery Council and General Medical Council. Openness and honesty when things go wrong: the professional duty of candour. 2015. http://www.gmc-uk.org/DoC_guidance_englsih.pdf_61618688.pdf. Accessed 16 Dec 2016.
Clinical Human Factors Group. The case of Elaine Bromiley. 2010. http://www.chfg.org/wp-content/uploads/2010/11/ElaineBromileyAnonymousReport.pdf. Accessed 3 Nov 2016.
Clinical Human Factors Group. Just a routine operation teaching video. 2012. http://chfg.org/learning-resources/just-a-routine-operation-teaching-video/. Accessed 3 Nov 2016.
Clinical Human Factors Group. About us: our history. Martin Bromiley. 2016. http://chfg.org/about-us/. Accessed 3 Nov 2016.
World Health Organization. Reporting and learning systems for medication errors: the role of pharmacovigilance centres. http://apps.who.int/iris/bitstream/10665/137036/1/9789241507943_eng.pdf?ua=1. Accessed 22 Dec 2016.
Reason J. Understanding adverse events: human factors. Qual Health Care. 1995;4:80–9.
Clinical Human Factors Group. What is human factors? 2016. http://chfg.org/about-us/what-is-human-factors/. Accessed 30 Oct 2016.
Scanlon M, Karsh B-T. The value of human factors to medication and patient safety in the ICU. Crit Care Med. 2010;38:S90–6.
Carayon P, Wetterneck TB, Cartmill R, et al. Characterizing the complexity of medication safety using a human factors approach: an observational study in two intensive care units. BMJ Qual Saf. 2014;23:56–65.
Pearson P, Steven A, Howe A, et al. Patient safety in health care professional educational curricula: examining the learning experience. 2009. http://www.birmingham.ac.uk/Documents/college-mds/haps/projects/cfhep/psrp/finalreports/PS030PSRPReportFINAL0609.pdf. Accessed 30 Oct 2016.
Nie Y, Li L, Duan Y, et al. Patient safety education for undergraduate medical students: a systematic review. BMC Med Educ. 2011;11:33. http://www.biomedcentral.com/1472-6920/11/33. Accessed 22 Dec 2016.
General Medical Council. First do no harm. Enhancing patient safety teaching in undergraduate medical education. 2015. http://www.gmc-uk.org/First_do_no_harm_patient_safety_in_undergrad_education_FINAL.pdf_62483215.pdf. Accessed 22 Dec 2016.
World Health Organisation. Multi-professional patient safety curriculum guide. Geneva: WHO; 2011. www.who.int/patientsafety/education/curriculum/tools-download/en/. Accessed 22 Dec 2016.
General Pharmaceutical Council. Future pharmacists: standards for the initial education and training of pharmacists. 2011. https://www.pharmacyregulation.org/sites/default/files/GPhC_Future_Pharmacists.pdf. Accessed 3 Nov 2016.
Royal College of Nursing. Patient safety and human factor. 2016. https://www.rcn.org.uk/clinical-topics/patient-safety-and-human-factors. Accessed 3 Nov 2016.
Royal College of Nursing. Guidance on safe nurse staffing levels in the UK. 2011. https://www.rcn.org.uk/professional-development/publications/pub-003860. Accessed 3 Nov 2016.
Royal College of Nursing. Response of the Royal College of Nursing to the Francis report. 2013. https://www.rcn.org.uk/professional-development/publications/pub-004476. Accessed 3 Nov 2016.
Nursing and Midwifery Council. Standards for pre-registration nursing education. 2010. https://www.nmc.org.uk/globalassets/sitedocuments/standards/nmc-standards-for-pre-registration-nursing-education.pdf. Accessed 3 Nov 2016.
Health Education North East. Faculty of Patient Safety. 2016. https://hee.nhs.uk/hee-your-area/north-east/our-work/research-innovation/faculty-patient-safety. Accessed 22 Dec 2016.
Madsen P, Dillon RL, Tinsley CH. Airline safety improvement through experience with near-misses: a cautionary tale. Risk Anal. 2016;36:1054–66.
World Health Organization. WHO global patient safety challenge—medication safety. http://www.who.int/patientsafety/challenge/en/. Accessed 17 Dec 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All authors CH, ICKW, JC-W, DT and SM declare that they have no conflict of interest and none of the authors received any financial assistance to conduct this current opinion review or for the preparation of the manuscript. No funding was received to prepare this article.
Rights and permissions
About this article
Cite this article
Huynh, C., Wong, I.C.K., Correa-West, J. et al. Paediatric Patient Safety and the Need for Aviation Black Box Thinking to Learn From and Prevent Medication Errors. Pediatr Drugs 19, 99–105 (2017). https://doi.org/10.1007/s40272-017-0214-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-017-0214-8