Abstract
Diabetes management relies on effective evidence-based advice that informs and empowers individuals to manage their health. Alongside other cornerstones of diabetes management, dietary advice has the potential to improve glycaemic levels, reduce risk of diabetes complications and improve health-related quality of life. We have updated the 2004 recommendations for the nutritional management of diabetes to provide health professionals with evidence-based guidelines to inform discussions with patients on diabetes management, including type 2 diabetes prevention and remission. To provide this update we commissioned new systematic reviews and meta-analyses on key topics, and drew on the broader evidence available. We have strengthened and expanded on the previous recommendations to include advice relating to dietary patterns, environmental sustainability, food processing, patient support and remission of type 2 diabetes. We have used the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach to determine the certainty of evidence for each recommendation based on findings from the commissioned and identified systematic reviews. Our findings indicate that a range of foods and dietary patterns are suitable for diabetes management, with key recommendations for people with diabetes being largely similar for those for the general population. Important messages are to consume minimally processed plant foods, such as whole grains, vegetables, whole fruit, legumes, nuts, seeds and non-hydrogenated non-tropical vegetable oils, while minimising the consumption of red and processed meats, sodium, sugar-sweetened beverages and refined grains. The updated recommendations reflect the current evidence base and, if adhered to, will improve patient outcomes.
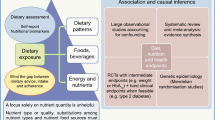
Graphical abstract

Similar content being viewed by others
Introduction
Diabetes management, including the prevention and remission of type 2 diabetes, relies on effective evidence-based advice that informs and empowers individuals to manage their health. Well-designed dietary recommendations and nutrition therapy are essential to improve both life expectancy and quality. However, the flood of nutrition information available is of variable quality, creates controversy regarding the best approaches, and is likely to confuse both people with diabetes and health professionals.
These new dietary recommendations for diabetes management have been produced by the Diabetes and Nutrition Study Group (DNSG) of the European Association for the Study of Diabetes (EASD). The recommendations are presented in short sections that often rely on detailed pre-published systematic reviews and meta-analyses commissioned by the DNSG and undertaken by separate groups with relevant expertise. The recommendations were finalised after presentations and extensive discussions within the DNSG. They are designed for health professionals, including those with and without dietetic training, who treat and advise people with diabetes, and replace the previous recommendations [1].
It is important to understand that dietary recommendations are written to provide guidance that is likely to benefit the majority of people with diabetes. They form a starting point for nutrition therapy, which all people with diabetes need and deserve. Achieving the best results for each individual patient also depends on the training and interpersonal skills of the health professional. As few people are able to make sudden, permanent or radical changes to their lifestyles, health professionals must judge and discuss with their patient how to apply these recommendations to obtain the greatest benefit for each person with diabetes.
This article is structured to provide evidence-based recommendations and commentary on macronutrients, foods, dietary patterns, and the broader lifestyle context of type 2 diabetes prevention and diabetes management. Recommendations for macronutrients and body weight are primarily derived from evidence pertaining to those with diabetes. Nutrient recommendations need to be applied in the context of what people eat, so recommendations for diabetes prevention, foods, dietary patterns and lifestyle are derived from broader populations that include those with diabetes. Details on the development of these recommendations is found within the electronic supplementary material (ESM) along with the AGREE Reporting Checklist [2]. We have used the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach to comment on the certainty of evidence for each recommendation based on findings from the commissioned systematic reviews. Certainty relates to the consistency of an observed effect, not the size of that effect. Each recommendation is graded as either ⊕⊝⊝⊝ very low, ⊕⊕⊝⊝ low, ⊕⊕⊕⊝ moderate or ⊕⊕⊕⊕ high, with very low certainty being the most likely to change over time as new research evidence emerges. This certainty of evidence determines how recommendations are worded. However, there is some variability in wording given the diversity in recommendations made. Recommendations should not be considered in isolation. Manufactured and composite foods considered to have beneficial attributes, such as a low-energy content, should only be recommended when their overall composition is consistent with recommendations for dietary fibre, sugars, saturated fat and protein. These recommendations do not include advice relating to several other topics important to nutrition advice, such as dietary sodium reduction to below 2000 mg, as these were deemed to be adequately covered elsewhere [3]. We believe these dietary recommendations reflect the current evidence base and will continue to be updated.
Prevention of type 2 diabetes

Commentary
Recommendations for type 2 diabetes prevention are based on meta-analyses of randomised controlled trials (RCTs) [4,5,6,7], as well as broader evidence relevant to diabetes prevention, including further systematic reviews and meta-analyses of prospective cohort studies [8,9,10], and large individual RCTs of intensive lifestyle interventions [11,12,13,14].
Type 2 diabetes prevalence is increasing worldwide. It is estimated that 537 million adults aged 20–79 years have diabetes, most of which is type 2 diabetes [15]. Strategies targeting both individuals at high risk and the general population are needed to curb the projected rise of type 2 diabetes to 783 million by 2045 [15]. To this end, the DNSG strongly emphasise the integral role and the importance of regional and nationwide health policy activities to curb the type 2 diabetes epidemic [16] and encourage establishing programmes for the prevention of type 2 diabetes in Europe and worldwide.
Lifestyle modification is a cornerstone of type 2 diabetes prevention. Intensive lifestyle interventions have been evaluated in several landmark RCTs in individuals of different ethnic groups who have overweight or obesity with an at-risk phenotype (mainly those with impaired glucose tolerance [IGT]) [4]. These interventions targeted 5–7% weight loss through energy-restricted healthy dietary patterns that are moderate in fat, low in saturated fat, and high in dietary fibre, whole grains, fruit, vegetables and legumes, and an increase in physical activity. The combination of dietary change and increased physical activity has been integral for sustained weight loss and reducing risk of type 2 diabetes incidence by 53% [4]. Weight loss through physical activity alone has not been as widely effective.
There is an important long-term effect of intensive lifestyle interventions [4]. The post-intervention follow up of the Da Qing IGT and Diabetes Study showed beneficial effects on reduced type 2 diabetes, microvascular complications, total cardiovascular disease (CVD), cardiovascular mortality and all-cause mortality even after 30 years of follow up [11]. Similar long-term post-intervention benefits were reported in the Diabetes Prevention Program Outcome study, with reduced type 2 diabetes and microvascular complications (restricted to women and those that did not develop diabetes) at 15 years of follow up [13], and the Finnish Diabetes Prevention Study, with reduced type 2 diabetes at 13 years and reduced early retinopathy in a subgroup analysis up to 10 years after the intervention [12, 17]. The strength of our first recommendation is due to these remarkable findings and long-term follow up.
Although the epidemic of type 2 diabetes has clearly followed the rise in overweight and obesity, type 2 diabetes is heterogeneous with regard to its detailed phenotype and genotype, and no long-term prevention trials have examined lifestyle intervention effects in different phenotype or genotype groups or compared different dietary patterns according to the phenotype or genetic predisposition to type 2 diabetes. However, there is suggestive evidence from post hoc analyses of the prevention trials that lifestyle changes may overcome the genetic variability in risk of type 2 diabetes [18]. Several implementation trials carried out in the primary healthcare setting for people with high risk of type 2 diabetes tend to confirm the results obtained from controlled trials [19, 20]—that lifestyle change effectively reduces type 2 diabetes irrespective of genotype or phenotype.
Other dietary patterns and food-based approaches that do not primarily target weight loss have also been associated with reduced type 2 diabetes risk in syntheses of large prospective cohort studies and in the PREDIMED trial. These include Mediterranean [4, 21], Nordic [6] and vegetarian dietary patterns [22], or diets high in vegetables and fruit [9], whole grains [8, 23] and fibre [8], or low in glycaemic index and load [10]. In observational studies, the combination of three or more health-related low-risk lifestyle behaviours that include maintaining a healthy body weight, regular physical activity, smoking abstinence or cessation, and nil-to-light alcohol consumption (note, we do not recommend alcohol consumption at any level [24,25,26]) have been associated with a nearly 80% reduction in type 2 diabetes risk. Pooled analyses of large prospective cohort studies reveal an inverse linear dose–response gradient in which the addition of each low-risk lifestyle behaviour decreases the risk of type 2 diabetes in individuals at varying background risk for type 2 diabetes [7].
Energy-balance and weight management in diabetes management

Commentary
These recommendations for body weight and weight loss are supported by published systematic reviews undertaken to inform the DNSG [27, 28] and by broader evidence relevant to weight management for people with diabetes.
Body function and maintenance requires a continuous but variable supply of energy from fats, carbohydrates and protein [29, 30], either directly after absorption from a meal, or from energy that is surplus to immediate mealtime need, stored as fat in adipose tissue [29]. Excess stored energy and age are the primary drivers for type 2 diabetes onset [31]. As populations have gained weight more rapidly and at younger ages, age at diagnosis of type 2 diabetes has fallen while body fat and body mass index (BMI) at diagnosis have risen [32,33,34]. The key feature behind development of metabolic diseases mediated by weight gain and obesity appears to be accumulation of ectopic fat, presumably via genetic and/or epigenetic mechanisms [35], in vital organs (e.g. liver and pancreas), thereby impairing their function [36]. When BMI is relatively low and in groups with similar BMI, high waist circumference (>94 cm in men, >80 cm in women) indicates elevated ectopic fat accumulation and risk of type 2 diabetes [37, 38]. The amount of weight gain needed to precipitate type 2 diabetes varies widely between individuals, but is less among Asian and Indigenous people than among people of European origin [39].
Extensive and consistent evidence has shown that intentional or therapeutic weight loss reduces blood glucose in people with type 2 diabetes and also improves most other major cardiometabolic risk factors (blood pressure, lipid profile and inflammation) [40, 41]. Clinical guidelines have always asserted that weight loss and weight-loss maintenance, using a healthful nutrient-complete diet and physical activity promotion, are fundamental to type 2 diabetes management before introducing medication [42, 43]. Weight loss improves cardiometabolic risks and reduces medication load. Recently it has become clear that, at least early after diagnosis of type 2 diabetes, substantial weight loss can reverse the accumulation of ectopic fat in liver and pancreas, and reliably generate remission of type 2 diabetes (return to non-diabetic HbA1c, without taking glucose-lowering medication) [27, 36]. Within 6 years from diagnosis, over 80% of people with type 2 diabetes can achieve remission by losing >15 kg of body weight [44, 45]. The likelihood of achieving remission declines with time after diagnosis, but may still be possible for some individuals after 10–20 years [46].
Weight loss occurs, inevitably, when less energy is consumed than is used over a sustained time frame [30, 47]. Faster weight loss occurs with a greater energy imbalance. As body weight falls, metabolic rate also falls slightly. Energy expenditure can be boosted by a sustained increase in physical activity, however, the individual must usually consume a diet that contains less energy than previously consumed to maintain their weight loss [47].
Many diet types can be used successfully to reduce energy intake and produce weight loss [27]. Weight-management diets commonly exclude or minimise the intake of one macronutrient or food group, while avoiding a compensatory increase in energy intake from other dietary sources. Other weight-loss diets focus on reducing portion size, or on attempting to increase satiety and feelings of fullness from what is consumed. A systematic ‘umbrella’ review of published meta-analyses of studies comparing hypoenergetic diets for weight management in people with type 2 diabetes does not support any particular weight-loss diet over others (e.g. low-carbohydrate, high-protein, low-glycaemic index, Mediterranean, high-monounsaturated fatty acid [MUFA] or vegetarian diets) [27]. This evidence indicates that a variety of weight-loss diets can be used equally effectively for weight management with type 2 diabetes, provided they can be followed and meet recommendations for protein, fat, micronutrient and fibre intake.
The evidence indicates that low-, and ‘very low’- (<3500 kJ/day [<840 kcal/day]) energy diets, using total diet replacement formula diet products (replacing all meals) or partial liquid meal replacement products (replacing 1–2 meals per day) for the weight-loss phase, were most effective for weight loss and reduction of other cardiometabolic risk factors when compared with the results from self-administered food-based weight-loss diets [27, 28, 48]. The Look AHEAD trial also showed that highest adherence to meal replacements in the intervention group was associated with an approximately fourfold greater odds of achieving the ≥7% weight-loss goal at 1 year [49]. However, many people find very-low-energy diets (1750–2300 kJ/day [420–550 kcal/day]) difficult to sustain, and they do not generate greater weight loss than formula diets providing ~3400 kJ/day (810 kcal/day) [48]. A step-down approach starting with 4200 kJ/day or 5000 kJ/day (1000–1200 kcal/day) is commonly advocated with obesity. Although all diet types are similarly effective for weight management, health risks could differ among weight-loss diets. For example, very-low-carbohydrate ketogenic diets have been associated with hypoglycaemia, ketoacidosis, and vitamin and mineral inadequacies, and both extreme high-carbohydrate and low-carbohydrate ketogenic diets have been associated with greater mortality [50,51,52,53,54,55,56].
Low-energy nutritionally complete formula diets with a ‘total diet replacement’ induction phase are the most effective dietary approach for achieving type 2 diabetes remission [27, 44, 57]. While short-term remission of type 2 diabetes is a striking and highly desirable outcome, the ultimate health benefits from weight management are likely to depend largely on long-term maintenance of a lower body weight. Long-term low-intensity structured programmes, including support for changing food choice, eating pattern and physical activity, and psychological support for behaviour change, can help to sustain new behaviours, relationships with foods and adherence to dietary advice, ultimately improving weight-loss maintenance [58, 59]. Consistent evidence is also accruing that long-term weight-loss maintenance is better after more rapid early weight loss [60]. Treatments effective for more rapid weight loss may thus have long-term value by sustaining motivation and adherence; however, benefits will be greatest with optimal weight-loss-maintenance strategy and support [45, 61]. Diet compositions for the weight-loss induction and maintenance phases need not necessarily be the same [47]. The choice of diet type depends on the skill and experience of the health professional supporting the patient, and on the enthusiasm of the person with diabetes for a particular diet type. Given that dietary adherence can be socially and psychologically testing, skills and empathy from the health professional is needed, providing consistent, long-term, evidence-based support [62]. As with all healthcare, patient preferences, culture, context and lifestyle consideration will require open conversation and shared decision-making between health professionals and people with diabetes.
Intensive lifestyle intervention combining both diet and physical activity (when possible) have been shown to benefit weight loss and reduce downstream complications. The Look AHEAD trial [63,64,65,66,67,68] used partial meal replacement for weight-loss induction combined with heavily supported physical activity training (moderate-intensity, 175 min per week). Those in the intervention achieved an overall weight loss of 8.6% vs 0.7% at 1 year, and 6.0% vs 3.5% at 9.6 years in completers from the intervention group (vs the control group). In those who achieved at least 10% weight loss, glycaemic levels and other cardiometabolic risk factors improved, with reduced incidence of major adverse cardiovascular events [64], nephropathy, non-alcoholic fatty liver disease (NAFLD), obstructive sleep apnoea and depression [63,64,65,66,67,68]. Diets prescribed for weight loss or long-term weight-loss maintenance need to be nutritionally complete, especially so when prescribed to older adults. Micronutrient supplements can also be prescribed if there is doubt that sufficient micronutrient intakes can be met. Anti-hyperglycaemic and antihypertensive medication use requires monitoring by health professionals before, during and after weight loss, so to reduce risk of hypoglycaemia and hypotension brought on by a reduced energy intake.
Carbohydrate intakes in diabetes management

Commentary
Recommendations based on carbohydrate amount, dietary fibre, NNS and glycaemic index are supported by published systematic reviews and meta-analyses commissioned by the DNSG [69,70,71,72,73]. The recommendation for carbohydrate counting is based on a recent systematic review [74] and the recommendation for free or added sugars is based on existing published systematic reviews and meta-analyses [75] and a World Health Organization (WHO) guideline [76] considered relevant to diabetes management.
Given that a wide range of carbohydrate intakes can be acceptable in diabetes management [69], these recommendations focus on carbohydrate quality, with the primary marker of quality being the amount of dietary fibre consumed. Diets high in naturally occurring fibre have been shown to be protective against cardiometabolic disease and premature mortality [8, 70]. Increasing fibre intakes can improve blood glucose and cholesterol levels and body weight, improving diabetes management [70]. The largest benefits in relation to glycaemic levels have been observed when moving from low to moderate or high fibre intakes. Those with diabetes, IGT or impaired fasting glucose should consume at least 35 g of fibre per day [70]. Beneficial effects have also been noted with lower and, for some people, more acceptable amounts [70].
Foods naturally high in dietary fibre are whole grains, vegetables, legumes, seeds, nuts and whole fruit. There is no indication that relatively high intakes of fibre-rich carbohydrate foods are associated with poor glycaemic levels or weight gain [77,78,79,80]. Basing a diet around high-fibre foods appears appropriate as such foods are also good sources of micronutrients, such as folate, non-haem iron and thiamine [81]. When choosing high-fibre foods, focus should be on minimally processed and largely intact whole grains, rather than products with finely milled whole grains that may also have added sugars, sodium and saturated fats. Processing and milling whole grains appear to lower their capacity to reduce glycaemic levels [82,83,84]. The same can be said of fruits, where whole and cut fruit are preferred over those that have been preserved in sweetened syrups, added to processed foods as a concentrate, or fruit juices [85]. As there was no difference between the benefits obtained from fibre-rich foods and fibre supplements in controlled trials of adults with IGT or impaired fasting glucose, type 1 diabetes or type 2 diabetes [70], some dietary fibre supplements appear a suitable method to obtain 35 g per day of fibre when sufficient fibre cannot be obtained from the diet alone.
Other markers of carbohydrate quality beyond fibre may also provide guidance in diabetes management, provided recommendations for added sugars, sodium and saturated fats are met [3, 76]. This is particularly relevant for manufactured and composite foods, which may be marketed based on one attribute (e.g. low in sugar) while not meeting other recommendations. Following a low-glycaemic index or -glycaemic load diet can improve glycaemic levels and intermediate cardiometabolic risk factors in those with diabetes [71]. High sugar intakes, especially from sugar-sweetened beverages at intakes of ≥10% of total energy, increase body weight [76, 86], fasting glucose and insulin [75], triacylglycerols [87] and uric acid [88] in people with or at risk for diabetes. High sugar intakes are also associated with increased risk of the metabolic syndrome [89], hypertension [90], gout [91] and CVD [92] in participants inclusive of people with or at risk for diabetes. For those looking to reduce free or added sugar intake, replacement with NNS may be an appropriate strategy. Non-nutritive-sweetened beverages, when replacing sugar-sweetened beverages, reduce body weight and cardiometabolic risk factors in people with or at risk for diabetes [72] and are associated with reductions in the risk of obesity and cardiovascular outcomes in participants inclusive of people with diabetes [73], with reductions similar to those seen with the standard of care, water.
Carbohydrate counting is a way of adjusting insulin dose to the amount of carbohydrate in a meal. The goal of carbohydrate counting in the treatment of type 1 and type 2 diabetes with a basal-bolus insulin regimen is to allow flexibility in meal choice by adjusting insulin dose to food intake without a negative effect on metabolic control and health outcomes. Carbohydrate counting may be useful as a technique for determining mealtime insulin dose in people with type 1 diabetes. Carbohydrate counting has been associated with improved HbA1c in adults, with no detrimental effect on severe hypoglycaemia or quality of life [74].
The habitual diets of individuals in Europe provide between 45% and 55% of total energy from carbohydrate. Definitions used for ‘low(er)’ and ‘high(er)’ carbohydrate diets vary greatly within the literature. They may refer to grams consumed per day, or the proportion of dietary energy from carbohydrate (% of total energy). Many studies examining ‘low(er)’ carbohydrate diets refer to <40% of total energy, while very-low-carbohydrate diets can be <30% of total energy or stricter. Meta-analyses have shown that when nutrient-complete low-carbohydrate diets are compared head-to-head, they are equally effective as higher carbohydrate (low-fat) diets, without any clinically significant long-term differences in glycaemic levels, lipids, blood pressure or weight management [69, 93,94,95]. A meta-analysis of trials in people with type 2 diabetes also showed that replacing carbohydrates with monounsaturated fats does improve glycaemic levels, blood lipids and systolic blood pressure, as well as reducing body weight [96]. Such findings fit with data from interventions promoting plant-based low-carbohydrate diets [97].
Use of extreme very-low-carbohydrate diets (ketogenic diets) is not recommended due to a lack of observed benefit in type 2 diabetes prevention and management, and due to potential safety concerns. Extreme carbohydrate restriction has been associated with increased low-density lipoprotein (LDL) cholesterol levels [69, 98], hypoglycaemia, ketoacidosis, and vitamin and mineral inadequacies [50,51,52,53,54,55,56]. These diets are difficult to follow in the long run [69] and there is lack of evidence on long-term effects [99]. Evidence from long-term observational studies in the general population indicates that low (<40% total energy) and high (>70% total energy) intakes of carbohydrate are associated with greater premature mortality [100,101,102,103]. If people with diabetes themselves choose to reduce carbohydrate to very low intakes, it is important this is done with health professional support [104] to ensure that micronutrient and fibre intakes remain adequate, and saturated fat intake is not increased above 10% of total energy intake [105]. Providing patient education on beneficial sources of carbohydrates (from whole grains, vegetables, fruit and legumes) and fat (unsaturated rather than saturated) is highly recommended.
Dietary fat intakes in diabetes management

Commentary
Recommendations based on dietary fats are supported by a published systematic review and meta-analysis commissioned by the DNSG [106] or from other recent reviews [107,108,109], and WHO guidelines [105] aimed at the general population but considered relevant to people with diabetes.
Dietary fats are present in or added to many foods in the food supply, however the influence on health depends on their constituent fatty acids. Our recommendations and those for the general population promote the consumption of foods containing primarily plant-based mono- and polyunsaturated fats, rather than saturated or trans-fats. This may be achieved by using non-hydrogenated non-tropical vegetable oils (e.g. olive oil, rapeseed/canola oil, soybean oil, sunflower oil, linseed oil) and through the consumption of seeds, nuts, fish and avocado, while limiting fats from meats and processed meats, butter, coconut products or palm oil.
Our recommendation is that total saturated fat intake is less than 10% total energy. The reduction of saturated fats in the diet is recommended mainly due to their potential to elevate LDL-cholesterol concentrations, which exhibit a causal relationship with atherogenesis and CVD [108, 110, 111]. Although there may be differences in the relationship between individual saturated fatty acids and CVD risk markers these are not apparent when considering clinical outcomes. Furthermore, different types of saturated fats often occur in the same foods. Thus, it seems appropriate that recommendations promote the reduction of total saturated fats. While the food matrix may play a potential role in the association between saturated fat intake and blood lipid levels [112], there is insufficient evidence on this topic to inform recommendations.
Our recommendation is that total trans-fats intake is less than 1% total energy. There is some evidence that an association between trans-fats and coronary heart disease (CHD) incidence may be due to the intake of industrially produced trans-fat rather than those naturally present in ruminant fat [113]. However, given the very small intakes of ruminant-derived trans-fats reported in most cohort studies, it is not possible to rule out potential harm associated with their intake. For this reason, it appears appropriate that current recommendations promote a reduction of total trans-fats [114]. Country regulatory efforts against partially hydrogenated fat use by the food industry have proved to be useful in reducing population intakes of trans-fats [114].
When reducing saturated and trans-fats in the diet, our recommendation is that, if replaced, it be with plant-based polyunsaturated and monounsaturated fats. In addition to improvements in blood lipids being associated with replacement of saturated fats by unsaturated fats [106, 108, 115], systematic reviews of randomised trials that included some participants with diabetes have identified additional cardiometabolic benefits with such substitutions [107, 116]. Replacing saturated fats with polyunsaturated fats results in reductions of HbA1c, fasting glucose concentration and liver fat content and improved Homeostatic Model Assessment of insulin resistance (HOMA-IR) [107]. Replacement with monounsaturated fats from primarily vegetable sources is also associated with improved HbA1c and HOMA-IR [107]. Although the evidence appears somewhat stronger for replacing saturated fats with polyunsaturated rather than monounsaturated fats, these fats are found in the same food sources such as a vegetable oils, nuts and seeds. Plant-based monounsaturated fats should provide the largest proportion of total dietary fat. With regard to the nature of polyunsaturated fats, those containing both n-6 and n-3 fatty acids should be recommended, with the larger proportion from sources rich in n-6 fatty acids.
Saturated fats may also be replaced in the diet with higher intakes of high-fibre foods [117] such as vegetables, whole grains, legumes and whole fruit, as discussed in our carbohydrate recommendations. Such dietary changes are likely to increase the polyunsaturated:saturated fatty acid ratio, which has also been associated with a reduction in CVD risk [106]. Importantly, saturated fat should not be replaced with rapidly digested carbohydrates such as sugars and simple starches [118].
Replacing foods high in saturated fats with foods and vegetable oils containing unsaturated fats (e.g. olive oil and rapeseed/canola oil) or high-fibre foods is likely to be beneficial in terms of promoting healthy eating habits [119] and aligns with broader dietary recommendations promoting food sources of unsaturated fatty acids. Nuts, including peanuts, are high in unsaturated fats, with evidence from cardiovascular outcomes trials indicating that mixed nuts (30 g/day) added to a Mediterranean dietary pattern reduces major cardiovascular events [120]. Data from prospective cohort studies indicate total nut intake is associated with reductions in total CVD and CVD mortality, CHD and CHD mortality, stroke mortality and atrial fibrillation in studies including some people with diabetes [121].
The evidence for use of n-3 supplements in diabetes treatment has shown no or little benefit for CVD reduction [116] There is, however, some support for recommending regular consumption of fatty fish as an additional means of reducing CHD risk in people with diabetes [122]. For those who are overweight or obese, reducing saturated fats (e.g. butter, cookies, cakes) without replacement may be a useful strategy for reducing energy intake.
Protein intakes in diabetes management

Commentary
Recommendations for protein intakes are supported by a published systematic review and meta-analysis commissioned by the DNSG in those with diabetes [123] and supported by a systematic review in people without diabetes [124].
There are two schools of thought concerning protein intake. Both low-protein diets and high-protein diets have been advocated. Protein intakes >20% of total energy have not been studied long term in people with type 2 diabetes. For this reason, we do not recommend high-protein diets (>20% total energy) over extended periods, unless when following an energy-reduced diet for weight loss. Meanwhile an intake below 10% total energy risks protein deficiency. Older people may require higher protein intakes (≥15% total energy) to maintain muscle mass and avoid sarcopenia [125, 126]. Studies in people with moderate to severe kidney disease (eGFR <60 ml/min per 1.73m2, i.e. stage 3a or less) are very limited. Evidence that high protein intake accelerates the loss of kidney function in people with diabetes is not consistently observed. For the present, therefore, we recommend protein intake should be in the lower normal range.
Energy-reduced weight-loss diets have been extensively studied and high-protein diets are frequently recommended for weight loss and to try to minimise loss of muscle mass. The meta-analyses on protein intakes of adults with type 2 diabetes participating in randomised prospective studies indicate moderate advantages with higher protein intakes, these being reductions of body weight, systolic and diastolic blood pressures and fasting blood glucose [123]. Kidney function was not adversely affected in studies up to 2 years post increase in protein intake in adults with type 2 diabetes and moderate to normal function (eGFR >60 ml/min per 1.73m2) [123].
Good sources of protein in the diet are dairy and dairy substitutes, legumes with complementary whole grains, eggs, fish, poultry and lean meat. Insufficient evidence exists from clinical trials in people with type 2 diabetes to indicate preferential intake of either animal or plant protein. However, high animal protein diets may exceed recommendations for saturated fat intakes (<10% total energy), with serum cholesterol concentrations and markers of blood glucose control generally lower for diets higher in protein from plants [127, 128].
Food-based approaches in diabetes management

Commentary
Recommendations for food-based approaches are supported by systematic reviews and meta-analyses commissioned by the DNSG that included broader populations inclusive of those with diabetes or at risk for diabetes [70, 129, 130] as well as broader evidence on these foods and relevant outcomes [85, 131,132,133,134,135,136].
Whole grains
Whole grains are those that retain their bran, endosperm and germ in the same proportions as an intact grain, but may have been dehulled. Examples of common whole grains are brown rice, whole wheat, rye, oats and barley. Increasing intakes of whole grains (including replacing refined grains with whole grains) has been shown to improve glycaemic levels, cardiometabolic risk factors and body weight measures in those with type 1 diabetes, type 2 diabetes, and IGT or impaired fasting glucose [70]. Wholegrain intakes are beneficial in CVD and hypertension management [137], and decreasing incidence of type 2 diabetes (by 10–22%) and other noncommunicable disease or mortality outcomes [8]. Wholegrain products in the current food supply may be more processed with added sugars, sodium and saturated fats than in the past. Furthermore there is emerging evidence that processing and milling whole grains appears to lower their capacity to reduce glycaemia [82,83,84]. For this reason, we recommend the intake of minimally processed and largely intact whole grains, rather than products where finely milled whole grains have been added.
Whole vegetables and fruit
Higher intakes of vegetables and fruit remain a universal recommendation among food-based dietary recommendations. The available evidence from prospective cohort studies not restricted to people with diabetes indicates risk reductions of around 10% per 200 g of vegetables and fruit per day for CHD, stroke and total mortality, with smaller but still significant reductions for total CVD and cancer. Dose–response effects were apparent for most outcomes relating to intake of up to 800 g of vegetables and fruit per day [85] . Specific fruit and vegetables (citrus, apples and pears among fruit sources, and allium, carrots, cruciferous and green leafy vegetable sources) have shown inverse associations with total CVD, CVD mortality, CHD, CHD mortality, stroke, stroke mortality and all-cause mortality [85, 135]. Results of RCTs that included those with diabetes indicate reductions in systolic blood pressure with increased vegetable and fruit intake, [75] reduced HbA1c with increased intake of berries [136], and reduced fasting plasma glucose, systolic blood pressure, LDL-cholesterol and BMI for increased intake of fruit alone (especially berries) [75, 136]. Results from prospective observational studies indicated that for root vegetables the cooking method was a primary driver of type 2 diabetes occurrence and hypertension, with boiled and roasted potatoes showing no relationship, but fried and salted potatoes being positively associated with type 2 diabetes occurrence [138]. Similarly for juicing, the evidence for benefits for 100% fruit juice appears restricted to levels of intake obtainable from a single piece of fruit (≤150 ml) [89, 90]. While we recommend whole vegetable and fruit intake, the rapidly digestible starch and sugar provided by whole vegetables and fruit may need to be taken into consideration in people with diabetes if intakes are very high. In such situations, higher intakes of green leafy vegetables rather than root vegetables or intakes of temperate fruit such as berries (5g sugars/100g), citrus fruit (7–9g sugars/100g), and apples and pears (10g sugars/100g) may be useful.
Legumes
Legumes include pulses (e.g. beans, peas, chickpeas and lentils), oil-seed legumes (e.g. soy, peanuts) and fresh legumes (e.g. peas, string beans). Results from RCTs indicate reductions in markers of glycaemia (HbA1c and fasting blood glucose), established lipid targets (LDL-cholesterol, non-high-density lipoprotein [HDL]-cholesterol), systolic blood pressure and body weight [139] with pulses at median intakes of 120–132 g/day (0.5–0.75 cups/day) and reductions in total and LDL-cholesterol with soy at a median intake of soy protein of 25 g/day [131, 132]. The available evidence from large prospective cohort studies that included some participants with diabetes indicates legumes are associated with lower risk of total CVD, CHD and hypertension, and obesity incidence [129]. Type 2 diabetes incidence was not reduced by higher intake of legumes in meta-analyses [129, 140, 141].
Nuts and seeds
Nuts include tree nuts such as almonds, walnuts, pistachios, pecans, Brazil nuts, cashews, hazelnuts, macadamia nuts and pine nuts. Peanuts (an oil-seed legume) are also often included in assessments of nuts. Results of RCTs of intermediate risk factors indicate reductions in established lipid targets (LDL-cholesterol, total cholesterol, triacylglycerols) [133, 142, 143] and markers of glycaemia (HbA1c, fasting blood glucose) [144] at median intakes of 50–67 g/day, without the concern of an associated increase in obesity or increases in body weight or other measures of adiposity [134]. The available evidence from large RCTs of clinical events supplemented by prospective cohort studies not restricted to people with diabetes demonstrates that mixed nuts (30 g/day) added to a Mediterranean dietary pattern reduces major cardiovascular events [120] and total nut intake is associated with lower risk of total CVD and CVD mortality, CHD and CHD mortality, stroke mortality and atrial fibrillation [121]. While there is less evidence available on whole seed intakes, their comparable nutrient profile and place as an ingredient or snack implies a similar benefit with their intake as observed with nuts.
Traditional dietary patterns and therapeutic diets in diabetes management

Commentary
Traditional dietary patterns
Recommendations for traditional dietary patterns are derived from published systematic reviews and meta-analyses commissioned by the DNSG that included broader populations inclusive of those with diabetes or at risk for diabetes on the Mediterranean [145], Nordic [5] and vegetarian [146, 147] dietary patterns, as well as broader evidence relevant to dietary pattens for people with diabetes including further systematic reviews [142, 148, 149], RCTs [120, 142, 150,151,152] and prospective cohort studies [153,154,155].
Mediterranean dietary patterns
Mediterranean dietary patterns are characterised by high consumption of vegetables, legumes, whole grains, fruits, nuts and extra virgin olive oil, moderate consumption of fish and wine, and low consumption of red and processed meat, processed food and added sugars [156, 157]. Results from RCTs indicate reductions in fasting plasma glucose, body weight, LDL-cholesterol, triacylglycerols, blood pressure [142, 148] and reduced need for anti-hyperglycaemic medications [151, 152]. Retinopathy but not nephropathy was reduced in the randomised prospective PREDIMED Study [150]. Observational prospective studies not specific to, but including some people with diabetes indicate that Mediterranean dietary patterns reduce major cardiovascular events [120, 145] and CHD mortality [145], and are associated with further reductions in all-cause mortality [149], cardiovascular mortality, and stroke incidence and mortality [145]. In addition, in primary and secondary prevention CVD trials including a large proportion of participants with diabetes, the Mediterranean diet has demonstrated beneficial effects on CVD and mortality incidence [120, 158].
Nordic dietary patterns
Nordic dietary patterns, known variably as the Nordic diet [159], New Nordic Diet [160] the Healthy Nordic diet [161, 162] and Baltic Sea Diet [163], emphasise whole grains (especially rye, barley and oats), berries, other temperate fruit (especially apples, pears), vegetables (especially root, cruciferous), legumes, fish, nuts and rapeseed/canola oil (as the main fat sources), and low-fat dairy [160, 161, 163, 164]. RCTs were done in at-risk individuals but not specifically in people with diabetes. Results indicate reductions in LDL-cholesterol and other established lipid targets (non-HDL-cholesterol, apolipoprotein B) and cardiometabolic risk factors (insulin, body weight, BMI, and systolic and diastolic blood pressure) [5]. The available evidence from large prospective cohort studies not limited to people with diabetes indicates that Nordic dietary patterns are associated with lower risk of total CVD, CVD mortality, cancer mortality, CHD and stroke [5].
Vegetarian dietary patterns
Vegetarian dietary patterns exclude some or all animal foods, emphasising the consumption of fruit, vegetables, legumes and whole grains, and exclude meat, poultry or fish. Lacto-ovo vegetarian dietary patterns include dairy and eggs, while a vegan diet excludes all animal products. Results from RCTs of vegetarian dietary patterns indicate reductions in HbA1c, fasting plasma glucose, LDL-cholesterol, non-HDL-cholesterol, body weight, BMI and waist circumference in people with diabetes [146]. The available evidence from large prospective cohort studies not limited to people with diabetes demonstrates that vegetarian dietary patterns are associated with reductions in CHD incidence and CVD mortality [147].
Therapeutic diets
Although published systematic reviews and meta-analyses were commissioned by the DNSG [6, 165] for therapeutic dietary patterns, specific recommendations were not made.
The Dietary Approaches to Stop Hypertension (DASH) therapeutic diet
DASH dietary patterns, aimed primarily at blood pressure reduction, emphasise fruit, vegetables, fat-free or low-fat dairy, whole grains, nuts and legumes, and limit the intake of total and saturated fat, cholesterol, red and processed meats, sweets and added sugars, including sugar-sweetened beverages, in the context of sodium restriction. Results from RCTs not limited to people with diabetes indicate reductions in systolic and diastolic blood pressure as well as HbA1c, fasting plasma insulin, body weight, and total and LDL-cholesterol [6] (⊕⊕⊝⊝ Low to ⊕⊕⊕⊝ Moderate). The available evidence from large prospective cohort studies not limited to people with diabetes demonstrates that DASH dietary patterns are associated with reductions in the risk of total CVD, CHD and stroke [6] (⊕⊕⊝⊝ Low).
Portfolio therapeutic diet
The Portfolio dietary pattern or Dietary Portfolio is a plant-based dietary pattern that emphasises a portfolio of four cholesterol-lowering foods/components (nuts, plant protein from soy or other legumes, viscous soluble fibre, and plant sterols) plus high MUFA-containing vegetable oils, all of which have approved health claims for cholesterol or CHD-risk reduction in Canada, the USA and/or Europe [134, 166,167,168,169,170,171]. RCTs were done in at-risk individuals but not specifically in people with diabetes. Results indicate reductions in LDL-cholesterol concentration [165], as well as in other established lipid targets (concentrations of total and non-HDL-cholesterol, triacylglycerols and apolipoprotein B), cardiometabolic risk factors (systolic and diastolic blood pressure, C-reactive protein [CRP]) (⊕⊕⊕⊝ Moderate to ⊕⊕⊕⊕ High), and in estimated 10 year CHD risk [165] (⊕⊝⊝⊝ Very low). These effects in people without diabetes were supported by a non-randomised study conducted in people with type 2 diabetes and CHD who were placed on statin therapy for 6 weeks [172]. Associated reductions in HbA1c, fasting glucose, triacylglycerols, waist circumference and BMI have also been shown [155]. The available evidence from large prospective cohort studies not limited to people with diabetes indicates that Portfolio dietary patterns are associated with reductions in total CVD, CHD, chronic heart failure [153], cancer mortality and all-cause mortality [154], with no interaction by diabetes status in subgroup analyses.
Environmental sustainability and diabetes management
Sustainable diets are those that contribute to food and nutrition security for present and future generations and have the lowest possible environmental impact. As with recommendations for the general population, it is important that recommendations for people with diabetes acknowledge the environmental consequences of promoting certain foods, nutrients and dietary patterns [173]. Given the considerable variation in environmental emissions, such as carbon dioxide, associated with the production of some foods [174], it is our intention that these recommendations be in line with food systems that support planetary health.
Our recommendations encourage intakes of plant-based and minimally processed foods, and the restriction of free sugars, sodium and saturated fats. As well as improving health, plant-based and minimally processed foods are considered to have the lowest environmental impact [175, 176]. Diets based on such foods that promote health and have a low environmental impact can support sustainable diets in Europe and in other countries that use these recommendations to inform their dietary recommendations for diabetes management.
A wide range of supportive initiatives are required to promote sustainable diets at the individual and household level. These include approaches to reduce food waste [177] and single-use plastics [178]. As our understanding of sustainability grows, so will its importance in protecting planetary health [179] and shaping sustainable dietary recommendations of the future.
Food processing and diabetes management
Virtually all foods have undergone some processing, even if just washing or peeling. Processing is important to preserve food by reducing microbial spoilage or oxidative degradation [81]. Historically, processing to extend the lifespan of the food used inorganic additives, such as salt or sodium nitrite, which have potentially hazardous effects for consumers. Organic preservatives are now usual for manufactured foods, with other techniques also being used, such as freezing, which is a harmless alternative and preserves the nutrients in foods. Food processing now is also undertaken to enhance the commercial value of foods, by altering their appearance and flavour, or by making them easier to prepare for consumption. Processing methods may add artificial ingredients and also remove natural components of foods. Food processing to ensure food safety as well as enhance the appeal of foods is now commonplace; however, the effects of food processing on the overall energy and nutrient intake of the diet requires further research.
Ultra-processed foods are foods that no longer resemble their native ingredients. Instead, they are manufactured through a series of industrial processes by combining substances derived from foods with additives [180]. Ultra-processed foods may be high in energy density, added sugars, sodium, and saturated and trans-fatty acids, while being low in fibre, protein, micronutrients and phytochemicals. Examples of ultra-processed foods are sugar-sweetened beverages, chocolate, chicken nuggets, fries and chips, and sweetened breakfast cereals. Unfortunately, there are no scientific classification systems agreed upon to identify what foods may be minimally or ultra-processed, or the mechanisms by which many food-processing techniques may influence health. Recent surveying indicates intakes of ultra-processed foods are increasing [181] and that these are the primary source of dietary energy in high-income countries [182]. Observational evidence, which does not demonstrate causality, indicates that greater intakes of ultra-processed foods are associated with adverse health outcomes, including increased mortality, CHD, type 2 diabetes and certain cancers [183,184,185,186,187,188,189,190]. To date, there are very few randomised trials considering the effects of ultra-processed food consumption on health [191]. While this is an area of potential concern, a greater mechanistic understanding of the effects of ultra-processed food intake on health is needed before recommendations specific to these products can be developed. Our best current advice is to promote the consumption of minimally processed plant-based foods such as whole grains, vegetables, whole fruit, legumes, nuts, seeds and non-hydrogenated non-tropical vegetable oils, while minimising the consumption of meat (especially red and processed meat), sugar-sweetened beverages, sweets and refined grains.
Patient support and diabetes management
Nutrition therapy places a large responsibility on individuals with diabetes to self-manage, which can be seen as demanding [192]. Determining food quality, or the energy or carbohydrate content of meals, is inherently difficult, as is abandoning one’s routines and favourite foods. A key goal of successful nutrition therapy, therefore, is to empower people with diabetes with the tools and support to self-manage [193]. It is important that health professionals transform these evidence-based dietary recommendations into practical, applicable advice. Interventions that go beyond knowledge and attitudes, to skills and competencies, have shown improved diabetes outcomes [194].
Health professionals must help their patients to select the dietary approach that best aligns with their values, preferences and treatment goals, to allow them to achieve the greatest adherence over the long term. An individual’s values and preferences are informed by their social, cultural and personal norms, as well as their experiences with allergies, intolerances and gastrointestinal side effects, and the cost of foods. Other promoters and barriers may include culinary (e.g. ability and time to prepare foods), environmental (e.g. sustainability of diets) and moral (e.g. animal welfare) considerations. As adherence is one of the most important determinants for attaining the benefits of any diet, the promoters and barriers of adherence must be considered for each patient when deciding together the best dietary approach. There are many potential issues with these discussions, such as health professional’s lacking sufficient training in nutrition, or their communication being perceived as judging or blaming [195]. It is important that healthcare professionals are aware of their own attitudes towards food and body weight when delivering nutrition therapy. It is important to convey that the aim of dietary advice is to decrease future risk of complications and improve health-related quality of life.
Data availability
Data for these recommendations were obtained from systematic reviews and meta-analyses cited within the document.
Change history
24 April 2023
The author line was incorrect in the HTML version of this article.
Abbreviations
- DASH:
-
Dietary Approaches to Stop Hypertension
- DNSG:
-
Diabetes and Nutrition Study Group
- IGT:
-
Impaired glucose tolerance
- MUFA:
-
Monounsaturated fatty acids
- NNS:
-
Non-nutritive sweetener
References
Mann JI, De Leeuw I, Hermansen K et al (2004) Evidence-based nutritional approaches to the treatment and prevention of diabetes mellitus. Nutr Metab Cardiovasc Dis 14(6):373–394. https://doi.org/10.1016/S0939-4753(04)80028-0
Brouwers MC, Kerkvliet K, Spithoff K, AGREE Nexts Steps Consortium (2016) The AGREE Reporting Checklist: a tool to improve reporting of clinical practice guidelines. BMJ 352:i1152. https://doi.org/10.1136/bmj.i1152
World Health Organization (2012) Guideline: sodium intake for adults and children. World Health Organization, Geneva
Uusitupa M, Khan TA, Viguiliouk E et al (2019) Prevention of type 2 diabetes by lifestyle changes: a systematic review and meta-analysis. Nutrients 11(11):2611. https://doi.org/10.3390/nu11112611
Massara P, Viguiliouk E, Glenn A et al (2020) Nordic dietary pattern and cardiometabolic outcomes: a systematic review and meta-analysis of prospective cohort studies and randomized controlled trials. Curr Dev Nutr 4(Supplement_2):546–546
Chiavaroli L, Viguiliouk E, Nishi SK et al (2019) DASH dietary pattern and cardiometabolic outcomes: an umbrella review of systematic reviews and meta-analyses. Nutrients 11(2):338. https://doi.org/10.3390/nu11020338
Khan TA, Field D, Chen V et al (2023) Combination of multiple low-risk lifestyle behaviors and incident type 2 diabetes: a systematic review and dose-response meta-analysis of prospective cohort studies. Diabetes Care 46(3):643–656. https://doi.org/10.2337/dc22-1024
Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L (2019) Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet 393(10170):434–445. https://doi.org/10.1016/S0140-6736(18)31809-9
Schwingshackl L, Hoffmann G, Lampousi A-M et al (2017) Food groups and risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol 32(5):363–375. https://doi.org/10.1007/s10654-017-0246-y
Livesey G, Taylor R, Livesey HF et al (2019) Dietary glycemic index and load and the risk of type 2 diabetes: a systematic review and updated meta-analyses of prospective cohort studies. Nutrients 11(6):1280. https://doi.org/10.3390/nu11061280
Li G, Zhang P, Wang J et al (2014) Cardiovascular mortality, all-cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: a 23-year follow-up study. Lancet Diabetes Endocrinol 2(6):474–480. https://doi.org/10.1016/S2213-8587(14)70057-9
Aro A, Kauppinen A, Kivinen N et al (2019) Life style intervention improves retinopathy status-The Finnish Diabetes Prevention Study. Nutrients 11(7):1691. https://doi.org/10.3390/nu11071691
Group Diabetes Prevention Program Research Group (2015) Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol 3(11):866–875. https://doi.org/10.1016/S2213-8587(15)00291-0
Uusitupa M, Peltonen M, Lindström J et al (2009) Ten-year mortality and cardiovascular morbidity in the Finnish Diabetes Prevention Study—secondary analysis of the randomized trial. PloS One 4(5):e5656. https://doi.org/10.1371/journal.pone.0005656
Sun H, Saeedi P, Karuranga S et al (2022) IDF Diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 183:109119. https://doi.org/10.1016/j.diabres.2021.109119
United Nations (2011) Political declaration of the high-level meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. 66th Session of the United Nations General Assembly. United Nations, New York, NY
Lindström J, Peltonen M, Eriksson J et al (2013) Improved lifestyle and decreased diabetes risk over 13 years: long-term follow-up of the randomised Finnish Diabetes Prevention Study (DPS). Diabetologia 56(2):284–293. https://doi.org/10.1007/s00125-012-2752-5
Uusitupa M, Lindström J, Tuomilehto J (2018) Prevention of type 2 diabetes—success story that is waiting for next steps. Eur J Clin Nutr 72(9):1260–1266. https://doi.org/10.1038/s41430-018-0223-x
Galaviz KI, Weber MB, Straus A, Haw JS, Narayan KV, Ali MK (2018) Global diabetes prevention interventions: a systematic review and network meta-analysis of the real-world impact on incidence, weight, and glucose. Diabetes Care 41(7):1526–1534. https://doi.org/10.2337/dc17-2222
Aziz Z, Absetz P, Oldroyd J, Pronk NP, Oldenburg B (2015) A systematic review of real-world diabetes prevention programs: learnings from the last 15 years. Implement Sci 10(1):1–17
Salas-Salvadó J, Bulló M, Estruch R et al (2014) Prevention of diabetes with Mediterranean diets: a subgroup analysis of a randomized trial. Ann Int Med 160(1):1–10. https://doi.org/10.7326/M13-1725
Qian F, Liu G, Hu FB, Bhupathiraju SN, Sun Q (2019) Association between plant-based dietary patterns and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA Int Med 179(10):1335–1344. https://doi.org/10.1001/jamainternmed.2019.2195
Pan X-R, Li G-W, Hu Y-H et al (1997) Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and Diabetes Study. Diabetes Care 20(4):537–544. https://doi.org/10.2337/diacare.20.4.537
Griswold MG, Fullman N, Hawley C et al (2018) Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 392(10152):1015–1035. https://doi.org/10.1016/S0140-6736(18)31310-2
Marlatt GA, Witkiewitz K (2002) Harm reduction approaches to alcohol use: health promotion, prevention, and treatment. Addict Behav 27(6):867–886. https://doi.org/10.1016/S0306-4603(02)00294-0
Nutt DJ, Rehm J (2014) Doing it by numbers: a simple approach to reducing the harms of alcohol. J Psychopharmacol 28(1):3–7. https://doi.org/10.1177/0269881113512038
Churuangsuk CHJ, Reynolds A, Griffin S, Combet E, Lean M (2022) Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission. Diabetologia 65(1):14–36. https://doi.org/10.1007/s00125-021-05577-2
Noronha JC, Nishi SK, Braunstein CR et al (2019) The effect of liquid meal replacements on cardiometabolic risk factors in overweight/obese individuals with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care 42(5):767–776. https://doi.org/10.2337/dc18-2270
Carreiro AL, Dhillon J, Gordon S et al (2016) The macronutrients, appetite, and energy intake. Annu Rev Nutr 36(1):73–103. https://doi.org/10.1146/annurev-nutr-121415-112624
Hall KD, Guo J (2017) Obesity energetics: body weight regulation and the effects of diet composition. Gastroenterology 152(7):1718–1727 e1713. https://doi.org/10.1053/j.gastro.2017.01.052
Kahn SE, Cooper ME, Del Prato S (2014) Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet 383(9922):1068–1083. https://doi.org/10.1016/S0140-6736(13)62154-6
World Health Organization (2021) Obesity and overweight. Available from: www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed: 4 August 2021
Koopman RJ (2005) Changes in age at diagnosis of type 2 diabetes mellitus in the United States, 1988 to 2000. Ann Fam Med 3(1):60–63. https://doi.org/10.1370/afm.214
Wilmot EG, Davies MJ, Yates T, Benhalima K, Lawrence IG, Khunti K (2010) Type 2 diabetes in younger adults: the emerging UK epidemic. Postgrad Med J 86(1022):711. https://doi.org/10.1136/pgmj.2010.100917
Hall LM, Moran CN, Milne GR et al (2010) Fat oxidation, fitness and skeletal muscle expression of oxidative/lipid metabolism genes in South Asians: implications for insulin resistance? PLoS One 5(12):e14197. https://doi.org/10.1371/journal.pone.0014197
Taylor R, Al-Mrabeh A, Zhyzhneuskaya S et al (2018) Remission of human type 2 diabetes requires decrease in liver and pancreas fat content but is dependent upon capacity for beta cell recovery. Cell Metab 28(4):547–556 e543. https://doi.org/10.1016/j.cmet.2018.07.003
Swainson MG, Batterham AM, Tsakirides C, Rutherford ZH, Hind K (2017) Prediction of whole-body fat percentage and visceral adipose tissue mass from five anthropometric variables. PLOS ONE 12(5):e0177175. https://doi.org/10.1371/journal.pone.0177175
Gautier A, Balkau B, Lange C, Tichet J, Bonnet F (2010) Risk factors for incident type 2 diabetes in individuals with a BMI of <27 kg/m2: the role of γ-glutamyltransferase. Data from an Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetologia 53(2):247–253. https://doi.org/10.1007/s00125-009-1602-6
Ntuk UE, Gill JM, Mackay DF, Sattar N, Pell JP (2014) Ethnic-specific obesity cutoffs for diabetes risk: cross-sectional study of 490,288 UK biobank participants. Diabetes Care 37(9):2500–2507. https://doi.org/10.2337/dc13-2966
Haase CL, Lopes S, Olsen AH, Satylganova A, Schnecke V, McEwan P (2021) Weight loss and risk reduction of obesity-related outcomes in 0.5 million people: evidence from a UK primary care database. Int J Obes 45(6):1249–1258. https://doi.org/10.1038/s41366-021-00788-4
Wing RR, Lang W, Wadden TA et al (2011) Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 34(7):1481–1486. https://doi.org/10.2337/dc10-2415
American Diabetes Association (2021) 8. Obesity management for the treatment of type 2 diabetes: standards of medical care in diabetes-2021. Diabetes Care 44(Suppl 1):S100–S110. https://doi.org/10.2337/dc21-S008
Dyson PA, Twenefour D, Breen C et al (2018) Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet Med 35(5):541–547. https://doi.org/10.1111/dme.13603
Lean ME, Leslie WS, Barnes AC et al (2018) Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet 391(10120):541–551. https://doi.org/10.1016/S0140-6736(17)33102-1
Lean MEJ, Leslie WS, Barnes AC et al (2019) Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol 7(5):344–355. https://doi.org/10.1016/S2213-8587(19)30068-3
Steven S, Hollingsworth KG, Al-Mrabeh A et al (2016) Very low-calorie diet and 6 months of weight stability in type 2 diabetes: pathophysiological changes in responders and nonresponders. Diabetes Care 39(5):808–815. https://doi.org/10.2337/dc15-1942
Hall KD, Kahan S (2018) Maintenance of lost weight and long-term management of obesity. Med Clin North Am 102(1):183–197. https://doi.org/10.1016/j.mcna.2017.08.012
Christensen P, Bliddal H, Riecke BF, Leeds AR, Astrup A, Christensen R (2011) Comparison of a low-energy diet and a very low-energy diet in sedentary obese individuals: a pragmatic randomized controlled trial. Clin Obes 1(1):31–40. https://doi.org/10.1111/j.1758-8111.2011.00006.x
Wadden TA, West DS, Neiberg RH et al (2009) One-year weight losses in the Look AHEAD study: factors associated with success. Obesity 17(4):713–722. https://doi.org/10.1038/oby.2008.637
Churuangsuk C, Griffiths D, Lean MEJ, Combet E (2019) Impacts of carbohydrate-restricted diets on micronutrient intakes and status: A systematic review. Obes Rev 20(8):1132–1147. https://doi.org/10.1111/obr.12857
Leow ZZX, Guelfi KJ, Davis EA, Jones TW, Fournier PA (2018) The glycaemic benefits of a very-low-carbohydrate ketogenic diet in adults with Type 1 diabetes mellitus may be opposed by increased hypoglycaemia risk and dyslipidaemia. Diabet Med 35(9):1258–1263. https://doi.org/10.1111/dme.13663
Spoke C, Malaeb S (2020) A case of hypoglycemia associated with the ketogenic diet and alcohol use. J Endocr Soc 4(6):bvaa045. https://doi.org/10.1210/jendso/bvaa045
Charoensri S, Sothornwit J, Trirattanapikul A, Pongchaiyakul C (2021) Ketogenic diet-induced diabetic ketoacidosis in a young adult with unrecognized type 1 diabetes. Case Rep Endocrinol 2021:6620832. https://doi.org/10.1155/2021/6620832
Marzban S, Arbee M, Vorajee N, Richards GA (2020) Non-diabetic ketoacidosis associated with a low carbohydrate, high fat diet in a postpartum lactating female. Oxf Med Case Rep 2020(8):omz026. https://doi.org/10.1093/omcr/omz026
Tougaard NH, Faber J, Eldrup E (2019) Very low carbohydrate diet and SGLT-2-inhibitor: double jeopardy in relation to ketoacidosis. BMJ Case Rep 12(4):e227516. https://doi.org/10.1136/bcr-2018-227516
White-Cotsmire AJ, Healy AM (2020) Ketogenic diet as a trigger for diabetic ketoacidosis in a misdiagnosis of diabetes: a case report. Clin Diabetes 38(3):318–321. https://doi.org/10.2337/cd20-0001
Thom G, Messow CM, Leslie W et al (2021) Predictors of type 2 diabetes remission in the Diabetes Remission Clinical Trial (DiRECT). Diabetic Med 38(8):e14395. https://doi.org/10.1111/dme.14395
Ismail K, Winkley K, Rabe-Hesketh S (2004) Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet 363(9421):1589–1597. https://doi.org/10.1016/S0140-6736(04)16202-8
American Diabetes Association (2021) 5. Facilitating behavior change and well-being to improve health outcomes: standards of medical care in diabetes-2021. Diabetes Care 44(Suppl 1):S53–S72. https://doi.org/10.2337/dc21-S005
Unick JL, Neiberg RH, Hogan PE et al (2015) Weight change in the first 2 months of a lifestyle intervention predicts weight changes 8 years later. Obesity 23(7):1353–1356. https://doi.org/10.1002/oby.21112
Lean M, Hankey C (2018) Keeping it off: the challenge of weight-loss maintenance. Lancet Diabetes Endocrinol 6(9):681–683. https://doi.org/10.1016/S2213-8587(17)30405-9
Dambha-Miller H, Day A, Kinmonth AL, Griffin SJ (2021) Primary care experience and remission of type 2 diabetes: a population-based prospective cohort study. Fam Pract 38(2):141–146. https://doi.org/10.1093/fampra/cmaa086
Group LAR (2013) Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 369(2):145–154. https://doi.org/10.1056/NEJMoa1212914
The Look AHEAD Research Group (2016) Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol 4(11):913–921. https://doi.org/10.1016/S2213-8587(16)30162-0
The Look AHEAD Research Group (2014) Effect of a long-term behavioural weight loss intervention on nephropathy in overweight or obese adults with type 2 diabetes: a secondary analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol 2(10):801–809. https://doi.org/10.1016/S2213-8587(14)70156-1
Lazo M, Solga SF, Horska A et al (2010) Effect of a 12-month intensive lifestyle intervention on hepatic steatosis in adults with type 2 diabetes. Diabetes Care 33(10):2156–2163. https://doi.org/10.2337/dc10-0856
Kuna ST, Reboussin DM, Borradaile KE et al (2013) Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep 36(5):641–649. https://doi.org/10.5665/sleep.2618
The Look AHEAD Research Group (2014) Impact of intensive lifestyle intervention on depression and health-related quality of life in type 2 diabetes: the Look AHEAD Trial. Diabetes Care 37(6):1544–1553. https://doi.org/10.2337/dc13-1928
Korsmo-Haugen HK, Brurberg KG, Mann J, Aas AM (2019) Carbohydrate quantity in the dietary management of type 2 diabetes: A systematic review and meta-analysis. Diabetes Obes Metab 21(1):15–27. https://doi.org/10.1111/dom.13499
Reynolds AN, Akerman AP, Mann J (2020) Dietary fibre and whole grains in diabetes management: Systematic review and meta-analyses. PLoS Med 17(3):e1003053. https://doi.org/10.1371/journal.pmed.1003053
Chiavaroli L, Lee D, Ahmed A et al (2021) Effect of low glycaemic index or load dietary patterns on glycaemic control and cardiometabolic risk factors in diabetes: systematic review and meta-analysis of randomised controlled trials. BMJ 374:n1651. https://doi.org/10.1136/bmj.n1651
McGlynn ND, Khan TA, Wang L et al (2022) Association of low- and no-calorie sweetened beverages as a replacement for sugar-sweetened beverages with body weight and cardiometabolic risk: a systematic review and meta-analysis. JAMA Netw Open 5(3):e222092. https://doi.org/10.1001/jamanetworkopen.2022.2092
Lee JJ, Khan TA, McGlynn N et al (2022) Relation of change or substitution of low-and no-calorie sweetened beverages with cardiometabolic outcomes: a systematic review and meta-analysis of prospective cohort studies. Diabetes Care 45(8):1917–1930. https://doi.org/10.2337/dc21-2130
Vaz EC, Porfírio GJM, Nunes HRDC, Nunes-Nogueira VDS (2018) Effectiveness and safety of carbohydrate counting in the management of adult patients with type 1 diabetes mellitus: a systematic review and meta-analysis. Arch Endocrinol Metab 62(3):337–345. https://doi.org/10.20945/2359-3997000000045
Choo VL, Viguiliouk E, Mejia SB et al (2018) Food sources of fructose-containing sugars and glycaemic control: systematic review and meta-analysis of controlled intervention studies. BMJ 363:k4644. https://doi.org/10.1136/bmj.k4644
World Health Organization (2015) Guidleine: sugars intake for adults and children. World Health Organization, Geneva
Sylvetsky AC, Edelstein SL, Walford G et al (2017) A high-carbohydrate, high-fiber, low-fat diet results in weight loss among adults at high risk of type 2 diabetes. J Nutr 147(11):2060–2066. https://doi.org/10.3945/jn.117.252395
Simpson HCR, Lousley S, Geekie M et al (1981) A high carbohydrate leguminous fibre diet improves all aspects of diabetic control. Lancet 317(8210):1–5. https://doi.org/10.1016/S0140-6736(81)90112-4
Anderson JW, Ward K (1979) High-carbohydrate, high-fiber diets for insulin-treated men with diabetes mellitus. Am J Clin Nutr 32(11):2312–2321. https://doi.org/10.1093/ajcn/32.11.2312
Lousley S, Jones D, Slaughter P, Carter R, Jelfs R, Mann J (1984) High carbohydrate-high fibre diets in poorly controlled diabetes. Diabetic Med 1(1):21–25. https://doi.org/10.1111/j.1464-5491.1984.tb01916.x
Truswell AS, Mann J (2017) Essentials of human nutrition. Oxford University Press, Oxford
Tosh SM, Chu Y (2015) Systematic review of the effect of processing of whole-grain oat cereals on glycaemic response. Br J Nutr 114(8):1256–1262. https://doi.org/10.1017/S0007114515002895
Reynolds AN, Mann J, Elbalshy M et al (2020) Wholegrain particle size influences postprandial glycemia in type 2 diabetes: a randomized crossover study comparing four wholegrain breads. Diabetes Care 43(2):476–479. https://doi.org/10.2337/dc19-1466
Åberg S, Mann J, Neumann S, Ross AB, Reynolds AN (2020) Whole-grain processing and glycemic control in type 2 diabetes: a randomized crossover trial. Diabetes Care 43(8):1717–1723. https://doi.org/10.2337/dc20-0263
Aune D, Giovannucci E, Boffetta P et al (2017) Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol 46(3):1029–1056. https://doi.org/10.1093/ije/dyw319
Sievenpiper JL, de Souza RJ, Mirrahimi A et al (2012) Effect of fructose on body weight in controlled feeding trials: a systematic review and meta-analysis. Ann Int Med 156(4):291–304. https://doi.org/10.7326/0003-4819-156-4-201202210-00007
Chiavaroli L, de Souza RJ, Ha V et al (2015) Effect of fructose on established lipid targets: a systematic review and meta-analysis of controlled feeding trials. J Am Heart Assoc 4(9):e001700. https://doi.org/10.1161/JAHA.114.001700
Ayoub-Charette S, Chiavaroli L, Liu Q et al (2021) Different food sources of fructose-containing sugars and fasting blood uric acid levels: a systematic review and meta-analysis of controlled feeding trials. J Nutr 151(8):2409–2421. https://doi.org/10.1093/jn/nxab144
Semnani-Azad Z, Khan TA, Mejia SB et al (2020) Association of major food sources of fructose-containing sugars with incident metabolic syndrome: a systematic review and meta-analysis. JAMA Netw Open 3(7):e209993. https://doi.org/10.1001/jamanetworkopen.2020.9993
Liu Q, Ayoub-Charette S, Khan TA et al (2019) Important food sources of fructose-containing sugars and incident hypertension: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc 8(24):e010977. https://doi.org/10.1161/JAHA.118.010977
Ayoub-Charette S, Liu Q, Khan TA et al (2019) Important food sources of fructose-containing sugars and incident gout: a systematic review and meta-analysis of prospective cohort studies. BMJ Open 9(5):e024171. https://doi.org/10.1136/bmjopen-2018-024171
Khan TA, Tayyiba M, Agarwal A et al (2019) Relation of total sugars, sucrose, fructose, and added sugars with the risk of cardiovascular disease: a systematic review and dose-response meta-analysis of prospective cohort studies. Mayo Clin Proc 94(12):2399–2414. https://doi.org/10.1016/j.mayocp.2019.05.034
Snorgaard O, Poulsen GM, Andersen HK, Astrup A (2017) Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Res Care 5(1):e000354. https://doi.org/10.1136/bmjdrc-2016-000354
Naude CE, Brand A, Schoonees A, Nguyen KA, Chaplin M, Volmink J (2022) Low-carbohydrate versus balanced-carbohydrate diets for reducing weight and cardiovascular risk. Cochrane Database Syst Rev Issue 1, Art. no.: CD013334. https://doi.org/10.1002/14651858.CD013334.pub2
Sainsbury E, Kizirian NV, Partridge SR, Gill T, Colagiuri S, Gibson AA (2018) Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract 139:239–252. https://doi.org/10.1016/j.diabres.2018.02.026
Qian F, Korat AA, Malik V, Hu FB (2016) Metabolic effects of monounsaturated fatty acid–enriched diets compared with carbohydrate or polyunsaturated fatty acid–enriched diets in patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care 39(8):1448–1457. https://doi.org/10.2337/dc16-0513
Jenkins DJ, Wong JM, Kendall CW et al (2009) The effect of a plant-based low-carbohydrate (“Eco-Atkins”) diet on body weight and blood lipid concentrations in hyperlipidemic subjects. Arch Int Med 169(11):1046–1054. https://doi.org/10.1001/archinternmed.2009.115
Jayedi A, Zeraattalab-Motlagh S, Jabbarzadeh B et al (2022) Dose-dependent effect of carbohydrate restriction for type 2 diabetes management: a systematic review and dose-response meta-analysis of randomized controlled trials. Am J Clin Nutr 116(1):40–56. https://doi.org/10.1093/ajcn/nqac06
Parry Strong A, Wright-McNaughten M, Weatherall M et al (2022) Very low carbohydrate (ketogenic) diets in type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Diabetes Obes Metab 24:2431–2442. https://doi.org/10.1111/dom.14837
Noto H, Goto A, Tsujimoto T, Noda M (2013) Low-carbohydrate diets and all-cause mortality: a systematic review and meta-analysis of observational studies. PloS One 8(1):e55030. https://doi.org/10.1371/journal.pone.0055030
Seidelmann SB, Claggett B, Cheng S et al (2018) Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. Lancet Public Health 3(9):e419–e428. https://doi.org/10.1016/S2468-2667(18)30135-X
Mazidi M, Katsiki N, Mikhailidis DP et al (2019) Lower carbohydrate diets and all-cause and cause-specific mortality: a population-based cohort study and pooling of prospective studies. Eur Heart J 40(34):2870–2879. https://doi.org/10.1093/eurheartj/ehz174
Churuangsuk C, Lean ME, Combet E (2020) Lower carbohydrate and higher fat intakes are associated with higher hemoglobin A1c: findings from the UK National Diet and Nutrition Survey 2008–2016. Eur J Nutr 59(6):2771–2782. https://doi.org/10.1007/s00394-019-02122-1
Muscogiuri G, El Ghoch M, Colao A, Hassapidou M, Yumuk V, Busetto L (2021) European guidelines for obesity management in adults with a very low-calorie ketogenic diet: a systematic review and meta-analysis. Obes Facts 14(2):222–245. https://doi.org/10.1159/000515381
World Health Organization (2018) Draft guidelines on saturated fatty acid and trans-fatty acid intake for adults and children. Available from: https://cdn.who.int/media/docs/default-source/nutritionlibrary/cfs-vgfsyn/draft-who-sfa-tfa-guidelines-public-consultation.pdf?sfvrsn=dc29c6af_5. Accessed: 30 September 2021
Schwab U, Reynolds AN, Sallinen T, Rivellese AA, Riserus U (2021) Dietary fat intakes and cardiovascular disease risk in adults with type 2 diabetes: a systematic review and meta-analysis. Eur J Nutr 60(6):3355–3363. https://doi.org/10.1007/s00394-021-02507-1
Imamura F, Micha R, Wu JH et al (2016) Effects of saturated fat, polyunsaturated fat, monounsaturated fat, and carbohydrate on glucose-insulin homeostasis: a systematic review and meta-analysis of randomised controlled feeding trials. PLoS Med 13(7):e1002087. https://doi.org/10.1371/journal.pmed.1002087
Mensink RP (2016) Effects of saturated fatty acids on serum lipids and lipoproteins: a systematic review and regression analysis. World Health Organization, Geneva
Hooper L, Martin N, Jimoh OF, Kirk C, Foster E, Abdelhamid AS (2020) Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst Rev Issue 8, Art. no.: CD011737. https://doi.org/10.1002/14651858.CD011737.pub3
Silverman MG, Ference BA, Im K et al (2016) Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA 316(12):1289–1297. https://doi.org/10.1001/jama.2016.13985
Ference BA, Ginsberg HN, Graham I et al (2017) Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J 38(32):2459–2472. https://doi.org/10.1093/eurheartj/ehx144
Rosqvist F, Smedman A, Lindmark-Månsson H et al (2015) Potential role of milk fat globule membrane in modulating plasma lipoproteins, gene expression, and cholesterol metabolism in humans: a randomized study. Am J Clin Nutr 102(1):20–30. https://doi.org/10.3945/ajcn.115.107045
Reynolds A, Hodson L, de Souza R, Tran Diep Pham H, Vlietstra L, Mann J (2023) Saturated fat and trans-fat intakes and their replacement with other macronutrients: a systematic review and meta-analysis of prospective observational studies. World Health Organization, Geneva
Wang S, Tian W, Liu Y et al (2021) Temporal trend of circulating trans-fatty acids and risk of long-term mortality in general population. Clin Nutr 40(3):1095–1101. https://doi.org/10.1016/j.clnu.2020.07.010
Schwab U, Lauritzen L, Tholstrup T et al (2014) Effect of the amount and type of dietary fat on cardiometabolic risk factors and risk of developing type 2 diabetes, cardiovascular diseases, and cancer: a systematic review. Food Nutr Res 58. https://doi.org/10.3402/fnr.v58.25145
Schulze MB, Minihane AM, Saleh RNM, Riserus U (2020) Intake and metabolism of omega-3 and omega-6 polyunsaturated fatty acids: nutritional implications for cardiometabolic diseases. Lancet Diabetes Endocrinol 8(11):915–930. https://doi.org/10.1016/S2213-8587(20)30148-0
Reiner Z, Catapano AL, De Backer G et al (2011) ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J 32(14):1769–1818. https://doi.org/10.1093/eurheartj/ehr158
Jakobsen MU, Dethlefsen C, Joensen AM et al (2010) Intake of carbohydrates compared with intake of saturated fatty acids and risk of myocardial infarction: importance of the glycemic index. Am J Clin Nutr 91(6):1764–1768. https://doi.org/10.3945/ajcn.2009.29099
Hirahatake KM, Jiang L, Wong ND et al (2019) Diet quality and cardiovascular disease risk in postmenopausal women with type 2 diabetes mellitus: The Women's Health Initiative. J Am Heart Assoc 8(19):e013249. https://doi.org/10.1161/JAHA.119.013249
Estruch R, Ros E, Salas-Salvadó J et al (2018) Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med 378(25):e34. https://doi.org/10.1056/NEJMoa1800389
Becerra-Tomás N, Paz-Graniel I, Hernández-Alonso P et al (2021) Nut consumption and type 2 diabetes risk: a systematic review and meta-analysis of observational studies. Am J Clin Nutr 113(4):960–971. https://doi.org/10.1093/ajcn/nqaa358
Hu FB, Cho E, Rexrode KM, Albert CM, Manson JE (2003) Fish and long-chain omega-3 fatty acid intake and risk of coronary heart disease and total mortality in diabetic women. Circulation 107(14):1852–1857. https://doi.org/10.1161/01.CIR.0000062644.42133.5F
Pfeiffer AFH, Pedersen E, Schwab U et al (2020) The effects of different quantities and qualities of protein intake in people with diabetes mellitus. Nutrients 12(2):365. https://doi.org/10.3390/nu12020365
Vogtschmidt YD, Raben A, Faber I et al (2021) Is protein the forgotten ingredient: effects of higher compared to lower protein diets on cardiometabolic risk factors. A systematic review and meta-analysis of randomised controlled trials. Atherosclerosis 328:124–135. https://doi.org/10.1016/j.atherosclerosis.2021.05.011
Bauer J, Biolo G, Cederholm T et al (2013) Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc 14(8):542–559. https://doi.org/10.1016/j.jamda.2013.05.021
Pedersen AN, Cederholm T (2014) Health effects of protein intake in healthy elderly populations: a systematic literature review. Food Nutr Res 58. https://doi.org/10.3402/fnr.v58.23364
Viguiliouk E, Stewart SE, Jayalath VH et al (2015) Effect of replacing animal protein with plant protein on glycemic control in diabetes: a systematic review and meta-analysis of randomized controlled trials. Nutrients 7(12):9804–9824. https://doi.org/10.3390/nu7125509
Li SS, Blanco Mejia S, Lytvyn L et al (2017) Effect of plant protein on blood lipids: A systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc 6(12):e006659. https://doi.org/10.1161/JAHA.117.006659
Viguiliouk E, Glenn AJ, Nishi SK et al (2019) Associations between dietary pulses alone or with other legumes and cardiometabolic disease outcomes: an umbrella review and updated systematic review and meta-analysis of prospective cohort studies. Adv Nutr 10(Supplement_4):S308–S319. https://doi.org/10.1093/advances/nmz113
Becerra-Tomás N, Paz-Graniel I, Kendall CWC et al (2019) Nut consumption and incidence of cardiovascular diseases and cardiovascular disease mortality: A meta-analysis of prospective cohort studies. Nutr Rev 77(10):691–709. https://doi.org/10.1093/nutrit/nuz042
Blanco Mejia S, Messina M, Li SS et al (2019) A meta-analysis of 46 studies identified by the FDA demonstrates that soy protein decreases circulating LDL and total cholesterol concentrations in adults. J Nutr 149(6):968–981. https://doi.org/10.1093/jn/nxz020
Jenkins DJ, Blanco Mejia S, Chiavaroli L et al (2019) Cumulative meta-analysis of the soy effect over time. J Am Heart Assoc 8(13):e012458. https://doi.org/10.1161/JAHA.119.012458
Sabaté J, Oda K, Ros E (2010) Nut consumption and blood lipid levels: a pooled analysis of 25 intervention trials. Arch Int Med 170(9):821–827. https://doi.org/10.1001/archinternmed.2010.79
Nishi SK, Viguiliouk E, Blanco Mejia S et al (2021) Are fatty nuts a weighty concern? A systematic review and meta-analysis and dose–response meta-regression of prospective cohorts and randomized controlled trials. Obes Rev 22(11):e13330. https://doi.org/10.1111/obr.13330
Zurbau A, Au-Yeung F, Blanco Mejia S et al (2020) Relation of different fruit and vegetable sources with incident cardiovascular outcomes: a systematic review and meta-analysis of prospective cohort studies. J Am Heart Assoc 9(19):e017728. https://doi.org/10.1161/JAHA.120.017728
Huang H, Chen G, Liao D, Zhu Y, Xue X (2016) Effects of berries consumption on cardiovascular risk factors: a meta-analysis with trial sequential analysis of randomized controlled trials. Sci Rep 6(1):1–11
Reynolds ANAA, Kumar S, Diep Pham HT, Coffey S, Mann J (2022) Dietary fibre in hypertension and cardiovascular disease management: systematic review and meta analyses. BMC Med 20(1):139. https://doi.org/10.1186/s12916-022-02328-x
Schwingshackl L, Schwedhelm C, Hoffmann G, Boeing H (2019) Potatoes and risk of chronic disease: A systematic review and dose–response meta-analysis. Eur J Nutr 58(6):2243–2251. https://doi.org/10.1007/s00394-018-1774-2
Viguiliouk E, Blanco Mejia S, Kendall CW, Sievenpiper JL (2017) Can pulses play a role in improving cardiometabolic health? Evidence from systematic reviews and meta-analyses. Ann N Y Acad Sci 1392(1):43–57. https://doi.org/10.1111/nyas.13312
Pearce M, Fanidi A, Bishop TRP et al (2021) Associations of total legume, pulse, and soy consumption with incident type 2 diabetes: federated meta-analysis of 27 studies from diverse world regions. J Nutr 151(5):1231–1240. https://doi.org/10.1093/jn/nxaa447
Ibsen DB, Steur M, Imamura F et al (2020) Replacement of red and processed meat with other food sources of protein and the risk of type 2 diabetes in European populations: The EPIC-InterAct Study. Diabetes Care 43(11):2660–2667. https://doi.org/10.2337/dc20-1038
Salas-Salvadó J, Becerra-Tomás N, García-Gavilán JF, Bullo M, Barrubes L (2018) Mediterranean diet and cardiovascular disease prevention: what do we know? Prog Cardiovasc Dis 61(1):62–67. https://doi.org/10.1016/j.pcad.2018.04.006
Blanco Mejia S, Kendall CWC, Viguiliouk E et al (2014) Effect of tree nuts on metabolic syndrome criteria: a systematic review and meta-analysis of randomised controlled trials. BMJ Open 4(7):e004660. https://doi.org/10.1136/bmjopen-2013-004660
Viguiliouk E, Kendall CWC, Blanco Mejia S et al (2014) Effect of tree nuts on glycemic control in diabetes: a systematic review and meta-analysis of randomized controlled dietary trials. PLOS ONE 9(7):e103376. https://doi.org/10.1371/journal.pone.0103376
Becerra-Tomás N, Blanco Mejía S, Viguiliouk E et al (2020) Mediterranean diet, cardiovascular disease and mortality in diabetes: a systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit Rev Food Sci Nutr 60(7):1207–1227. https://doi.org/10.1080/10408398.2019.1565281
Viguiliouk E, Kendall CW, Kahleová H et al (2019) Effect of vegetarian dietary patterns on cardiometabolic risk factors in diabetes: a systematic review and meta-analysis of randomized controlled trials. Clin Nutr 38(3):1133–1145. https://doi.org/10.1016/j.clnu.2018.05.032
Glenn AJ, Viguiliouk E, Seider M et al (2019) Relation of vegetarian dietary patterns with major cardiovascular outcomes: a systematic review and meta-analysis of prospective cohort studies. Front Nutr 6:80. https://doi.org/10.3389/fnut.2019.00080
Esposito K, Maiorino MI, Bellastella G, Chiodini P, Panagiotakos D, Giugliano D (2015) A journey into a Mediterranean diet and type 2 diabetes: a systematic review with meta-analyses. BMJ Open 5(8):e008222. https://doi.org/10.1136/bmjopen-2015-008222
Soltani S, Jayedi A, Shab-Bidar S, Becerra-Tomás N, Salas-Salvadó J (2019) Adherence to the Mediterranean diet in relation to all-cause mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Adv Nutr 10(6):1029–1039. https://doi.org/10.1093/advances/nmz041
Díaz-López A, Babio N, Martínez-González MA et al (2015) Mediterranean diet, retinopathy, nephropathy, and microvascular diabetes complications: a post hoc analysis of a randomized trial. Diabetes Care 38(11):2134–2141. https://doi.org/10.2337/dc15-1117
Esposito K, Maiorino MI, Ciotola M et al (2009) Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Int Med 151(5):306–314. https://doi.org/10.7326/0003-4819-151-5-200909010-00004
Basterra-Gortari FJ, Ruiz-Canela M, Martínez-González MA et al (2019) Effects of a Mediterranean eating plan on the need for glucose-lowering medications in participants with type 2 diabetes: a subgroup analysis of the PREDIMED trial. Diabetes Care 42(8):1390–1397. https://doi.org/10.2337/dc18-2475
Glenn AJ, Lo K, Jenkins DJ et al (2021) Relationship between a plant-based dietary portfolio and risk of cardiovascular disease: findings from the Women's Health Initiative Prospective Cohort Study. J Am Heart Assoc 10(16):e021515. https://doi.org/10.1161/JAHA.121.021515
Lo K, Glenn AJ, Yeung S et al (2021) Prospective association of the Portfolio diet with all-cause and cause-specific mortality risk in the Mr. OS and Ms. OS Study. Nutrients 13(12):4360. https://doi.org/10.3390/nu13124360
Glenn AJ, Hernández-Alonso P, Kendall CW et al (2021) Longitudinal changes in adherence to the portfolio and DASH dietary patterns and cardiometabolic risk factors in the PREDIMED-Plus study. Clin Nutr 40(5):2825–2836. https://doi.org/10.1016/j.clnu.2021.03.016
Willett WC, Sacks F, Trichopoulou A et al (1995) Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr 61(6):1402S–1406S. https://doi.org/10.1093/ajcn/61.6.1402S
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D (2003) Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 348(26):2599–2608. https://doi.org/10.1056/NEJMoa025039
Cano-Ibáñez N, Quintana-Navarro GM, Alcala-Diaz JF et al (2022) Long-term effect of a dietary intervention with two-healthy dietary approaches on food intake and nutrient density in coronary patients: results from the CORDIOPREV trial. Eur J Nutr 61(6):3019–3036. https://doi.org/10.1007/s00394-022-03006-7
Slimani N, Fahey M, Welch A et al (2002) Diversity of dietary patterns observed in the European Prospective Investigation into Cancer and Nutrition (EPIC) project. Public Health Nutr 5(6b):1311–1328. https://doi.org/10.1079/PHN2002407
Mithril C, Dragsted LO, Meyer C, Blauert E, Holt MK, Astrup A (2012) Guidelines for the New Nordic Diet. Public Health Nutr 15(10):1941–1947. https://doi.org/10.1017/S136898001100351X
Adamsson V, Reumark A, Cederholm T, Vessby B, Risérus U, Johansson G (2012) What is a healthy Nordic diet? Foods and nutrients in the NORDIET study. Food Nutr Res 56:18189. https://doi.org/10.3402/fnr.v56i0.18189
Adamsson V, Reumark A, Fredriksson I-B et al (2011) Effects of a healthy Nordic diet on cardiovascular risk factors in hypercholesterolaemic subjects: a randomized controlled trial (NORDIET). J Int Med 269(2):150–159. https://doi.org/10.1111/j.1365-2796.2010.02290.x
Kanerva N, Kaartinen NE, Schwab U, Lahti-Koski M, Männistö S (2014) The Baltic Sea Diet Score: a tool for assessing healthy eating in Nordic countries. Public Health Nutr 17(8):1697–1705. https://doi.org/10.1017/S1368980013002395
Uusitupa M, Hermansen K, Savolainen MJ et al (2013) Effects of an isocaloric healthy Nordic diet on insulin sensitivity, lipid profile and inflammation markers in metabolic syndrome – a randomized study (SYSDIET). J Intern Med 274(1):52–66. https://doi.org/10.1111/joim.12044
Chiavaroli L, Nishi SK, Khan TA et al (2018) Portfolio dietary pattern and cardiovascular disease: a systematic review and meta-analysis of controlled trials. Prog Cardiovasc Dis 61(1):43–53. https://doi.org/10.1016/j.pcad.2018.05.004
Health Canada (2010) Plant sterols and blood cholesterol lowering. Available from: www.canada.ca/en/health-canada/services/food-nutrition/food-labelling/health-claims/assessments/plant-sterols-blood-cholesterol-lowering-nutrition-health-claims-food-labelling.html. Accessed: 20 October 2022
Health Canada (2015) Summary of Health Canada’s Assessment of a Health Claim about Soy Protein and Cholesterol Lowering. Available from: www.canada.ca/en/health-canada/services/food-nutrition/food-labelling/health-claims/assessments/summary-assessment-health-claim-about-protein-cholesterol-lowering.html. Accessed: 20 October 2022
Health Canada (2021) List of dietary fibres reviewed and accepted by Health Canada’s Food Directorate. Available from: www.canada.ca/en/health-canada/services/publications/food-nutrition/list-reviewed-accepted-dietary-fibres.html. Accessed: 20 October 2022
US Food and Drug Administration (2022) Qualified health claims: letters of enforcement discretion. Available from: www.fda.gov/food/food-labeling-nutrition/qualified-health-claims-letters-enforcement-discretion. Accessed: 20 October 2022, DOI: https://doi.org/10.52628/88.4.07
EFSA (2006) Scientific Opinion on the substantiation of a health claim related to 3 g/day plant sterols/stanols and lowering blood LDL-cholesterol and reduced risk of (coronary) heart disease pursuant to Article 19 of Regulation (EC) No 1924/2006. Available from: www.efsa.europa.eu/en/efsajournal/pub/2693
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA) (2006) Scientific Opinion on the substantiation of a health claim related to oat beta glucan and lowering blood cholesterol and reduced risk of (coronary) heart disease pursuant to Article 14 of Regulation (EC) No 1924/2006. EFSA J 2010 8(12):1885. https://doi.org/10.2903/j.efsa.2010.1885
Keith M, Kuliszewski MA, Liao C et al (2015) A modified portfolio diet complements medical management to reduce cardiovascular risk factors in diabetic patients with coronary artery disease. Clin Nutr 34(3):541–548. https://doi.org/10.1016/j.clnu.2014.06.010
Tuomisto HL (2018) Importance of considering environmental sustainability in dietary guidelines. Lancet Planet Health 2(8):e331–e332. https://doi.org/10.1016/S2542-5196(18)30174-8
Vermeulen SJ, Campbell BM, Ingram JS (2012) Climate change and food systems. Ann Rev Environ Resour 37:195–222. https://doi.org/10.1146/annurev-environ-020411-130608
Willett W, Rockström J, Loken B et al (2019) Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 393(10170):447–492. https://doi.org/10.1016/S0140-6736(18)31788-4
Clark MA, Springmann M, Hill J, Tilman D (2019) Multiple health and environmental impacts of foods. Proc Natl Acad Sci 116(46):23357–23362. https://doi.org/10.1073/pnas.1906908116
Schanes K, Dobernig K, Gözet B (2018) Food waste matters - a systematic review of household food waste practices and their policy implications. J Clean Prod 182:978–991. https://doi.org/10.1016/j.jclepro.2018.02.030
UNEP (2018) Single-use plastics: a roadmap for sustainability. In. United Nations Environment Programme. Available from: www.unep.org/resources/report/single-use-plastics-roadmap-sustainability. Accessed: 20 October 2022
Horton R, Beaglehole R, Bonita R, Raeburn J, McKee M, Wall S (2014) From public to planetary health: a manifesto. Lancet 383(9920):847. https://doi.org/10.1016/S0140-6736(14)60409-8
Monteiro CA (2009) Nutrition and health. The issue is not food, nor nutrients, so much as processing. Public Health Nutr 12(5):729–731. https://doi.org/10.1017/S1368980009005291
Baker P, Machado P, Santos T et al (2020) Ultra-processed foods and the nutrition transition: global, regional and national trends, food systems transformations and political economy drivers. Obes Rev 21(12):e13126. https://doi.org/10.1111/obr.13126
Monteiro CA, Cannon G, Lawrence M, Costa Louzada MD, Pereira Machado P (2019) Ultra-processed foods, diet quality, and health using the NOVA classification system. FAO, Rome
Srour B, Fezeu LK, Kesse-Guyot E et al (2019) Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). BMJ 365:l1451. https://doi.org/10.1136/bmj.l1451
Narula N, Wong EC, Dehghan M et al (2021) Association of ultra-processed food intake with risk of inflammatory bowel disease: prospective cohort study. BMJ 374:n1554. https://doi.org/10.1136/bmj.n1554
Ivancovsky-Wajcman D, Fliss-Isakov N, Webb M et al (2021) Ultra-processed food is associated with features of metabolic syndrome and non-alcoholic fatty liver disease. Liver Int 41(11):2635–2645. https://doi.org/10.1111/liv.14996
Rico-Campà A, Martínez-González MA, Alvarez-Alvarez I et al (2019) Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ 365:l1949. https://doi.org/10.1136/bmj.l1949
Canella DS, Levy RB, Martins APB et al (2014) Ultra-processed food products and obesity in Brazilian households (2008–2009). PloS One 9(3):e92752. https://doi.org/10.1371/journal.pone.0092752
Monteiro CA, Moubarac J-C, Levy RB, Canella DS, da Costa Louzada ML, Cannon G (2018) Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr 21(1):18–26. https://doi.org/10.1017/S1368980017001379
Fiolet T, Srour B, Sellem L et al (2018) Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ 360:k322. https://doi.org/10.1136/bmj.k322
Chen X, Zhang Z, Yang H et al (2020) Consumption of ultra-processed foods and health outcomes: a systematic review of epidemiological studies. Nutr J 19(1):1–10
Hall KD, Ayuketah A, Brychta R et al (2019) Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab 30(1):67–77.e3. https://doi.org/10.1016/j.cmet.2019.05.008
Litterbach E, Holmes-Truscott E, Pouwer F, Speight J, Hendrieckx C (2020) 'I wish my health professionals understood that it's not just all about your HbA1c!'. Qualitative responses from the second Diabetes MILES–Australia (MILES-2) study. Diabetic Med 37(6):971–981. https://doi.org/10.1111/dme.14199
Rees S, Williams A (2009) Promoting and supporting self-management for adults living in the community with physical chronic illness: a systematic review of the effectiveness and meaningfulness of the patient-practitioner encounter. JBI Evid Synth 7(13):492–582. https://doi.org/10.11124/01938924-200907130-00001
Zare S, Ostovarfar J, Kaveh MH, Vali M (2020) Effectiveness of theory-based diabetes self-care training interventions; a systematic review. Diabetes Metab Syndr Clin Res Rev 14(4):423–433. https://doi.org/10.1016/j.dsx.2020.04.008
Liu NF, Brown AS, Folias AE et al (2017) Stigma in people with type 1 or type 2 diabetes. Clin Diabetes 35(1):27–34. https://doi.org/10.2337/cd16-0020
Acknowledgements
We are grateful to the DNSG members for their support during the guideline development process. Thank you to the EASD members who contributed to this document: Professor H. Klein, Professor R. Holt, Professor A. Tsapas, Professor A. Solini, Professor H. Hanaire and Professor D. Zozulińska-Ziółkiewicz. The graphical abstract was designed by Liane McGee (Fortyfive Design, Wellington, New Zealand).
Authors’ relationships and activities
Funding listed here is in addition to the funding specifically obtained to support the work behind this article. A-MA was funded by Oslo University Hospital, the University of Oslo, The Norwegian Directory of Health (scientific board and development of national diabetes guidelines) and The Norwegian Diabetes Association (advisor on nutrition and dietetics). A-MA has received grants or research support from Novo Nordisk Norway for development of an e-health programme for diabetes, the DAM foundation for research, Mills AS, and The Norwegian Diabetes Association for a research project investigating prebiotic fibres effect in type 2 diabetes. MA was funded by the University of Gothenburg, the Swedish Agency for Health Technology Assessment (SBU) and Oatly AB. CC was funded by the Prince of Songkla University, Thailand. CC has received grants or research support from the National Science, Research and Innovation Fund, Thailand. KH was funded by Aarhus University and the Danish Council on Health and Disease Prevention. KH has received grants or research support from the Danish Strategic Research Council and the Danish Innovation fund. CWCK was funded by the University of Toronto. CWCK has received grants or research support from the Advanced Food Materials Network, Agriculture and Agri-Foods Canada (AAFC), Almond Board of California, Barilla, Canadian Institutes of Health Research (CIHR), Canola Council of Canada, International Nut and Dried Fruit Council, International Tree Nut Council Research and Education Foundation, Loblaw Brands Ltd, the Peanut Institute, Pulse Canada and Unilever. CWCK has received in-kind research support from the Almond Board of California, Barilla, California Walnut Commission, Kellogg Canada, Loblaw Companies, Nutrartis, Quaker (PepsiCo), the Peanut Institute, Primo, Unico, Unilever, WhiteWave Foods/Danone. CWCK has received travel support and/or honoraria from Barilla, California Walnut Commission, Canola Council of Canada, General Mills, International Nut and Dried Fruit Council, International Pasta Organization, Lantmannen, Loblaw Brands Ltd, Nutrition Foundation of Italy, Oldways Preservation Trust, Paramount Farms, the Peanut Institute, Pulse Canada, Sun-Maid, Tate & Lyle, Unilever and White Wave Foods/Danone. CWCK has served on the scientific advisory board for the International Tree Nut Council, International Pasta Organization, McCormick Science Institute and Oldways Preservation Trust. CWCK is a founding member of the International Carbohydrate Quality Consortium (ICQC), Chair of the Diabetes and Nutrition Study Group (DNSG) of the European Association for the Study of Diabetes (EASD), is on the Clinical Practice Guidelines Expert Committee for Nutrition Therapy of the EASD and is a Director of Glycemia Consulting and the Toronto 3D Knowledge Synthesis and Clinical Trials foundation. HK was funded by the Physicians Committee for Responsible Medicine. TK was funded by the National Honey Board. TK has received grants or research support from the Canadian Institutes of Health Research (CIHR), National Honey Board, International Food Information Council (IFIC) and Institute for the Advancement of Food and Nutrition Sciences (IAFNS; formerly ILSI North America). MEJL was funded by the University of Glasgow. MEJL has received grants or research support from: Diabetes UK for DiRECT, DiRECT Extension, and DiRECT Economic evaluation; NIHR for ReDIRECT and iPREVENT; and All Saints Educational Trust for HoDIRECT Nepal. MEJL has received lecturing and consultancy fees from Novo Nordisk, Nestle, Oviva, Merck and Sanofi. JIM was funded by the Healthier Lives National Science Challenge of New Zealand. EP was funded by the University of Adelaide, CSIRO and the University of South Australia. AP was funded by the Charité Universitätsmedizin Berlin. AP has received grants or research support from EFSD/EASD, the German Center für Diabetes Research (DZD), the German Diabetes Foundation (DDS), Horizon EU, and the German Ministry for Science and Education. DR was funded by Vuk Vrhovac University Clinic, Merkur University Hospital and School of Medicine, and Catholic University of Croatia. DR has received grants or research support from Abbott, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly, Johnson & Johnson, Krka, Merck, MSD, Novartis, Novo Nordisk, Pliva, Roche, Sandoz, Sanofi, Salvus, Takeda and Viatris. ANR was funded by the Heart Foundation of New Zealand. ANR has received grants or research support from the Riddet Centre of Research Excellence, World Health Organization. UR was funded by Uppsala University and the Swedish Research Council FORMAS. UR has received grants or research support from the Swedish Diabetes Foundation, Excellence of Diabetes Research in Sweden and the Swedish Heart and Lung Foundation. AAR was funded by the University Federico II of Naples. JS-S was funded by the Rovira i Virgili University (Spain) and partially supported by the Catalan Institution for Research and Advanced Studies (ICREA) under the ICREA Academia programme. JS-S has received grants or research support from: Fondo de Investigaciones Sanitarias de la Seguridad Social, Instituto de salud Carlos III; CIBER Fisiopatología de la Obesidad y Nutrición, Instituto de Salud Carlos III; Agència de Gestió d'Ajuts Universitaris i de Recerca de la generalitat de Catalunya; Fundació Marató de TV3, Catalonia; and the International Nut and Dried Fruit Council (INC) Foundation through his institution (IISPV). JS-S received olive oil, pistachios and almonds from the Patrimonio Comunal Olivarero (Spain), Pistachio Growers of California (USA) and Almond Board of California (USA), respectively, for the PREDIMED-Plus study participants. JS-S received consulting fees or travel expenses from Instituto Danone Spain, the International Nut and Dried Fruit Foundation and Mundipharma laboratories Spain. US was funded by the University of Eastern Finland. JLS was funded by the University of Toronto and Province of Ontario through the Ontario Health Insurance Plan, and is or was funded by a PSI Graham Farquharson Knowledge Translation Fellowship, Diabetes Canada Clinician Scientist award, Canadian Institutes of Health Research (CIHR) INMD/CNS New Investigator Partnership Prize, and Banting & Best Diabetes Centre Sun Life Financial New Investigator Award. JLS has received grants or research support from Canadian Foundation for Innovation, Ontario Research Fund, Province of Ontario Ministry of Research and Innovation and Science, Canadian Institutes of Health Research (CIHR), Diabetes Canada, American Society for Nutrition (ASN), International Nut and Dried Fruit Council (INC) Foundation, National Honey Board (US Department of Agriculture [USDA] honey “Checkoff” programme), Institute for the Advancement of Food and Nutrition Sciences (IAFNS; formerly ILSI North America), Pulse Canada, Quaker Oats Center of Excellence, The United Soybean Board (USDA soy “Checkoff” programme), The Tate and Lyle Nutritional Research Fund at the University of Toronto, The Glycemic Control and Cardiovascular Disease in Type 2 Diabetes Fund at the University of Toronto (a fund established by the Alberta Pulse Growers), The Plant Protein Fund at the University of Toronto (a fund which has received contributions from IFF), and The Nutrition Trialists Network Fund at the University of Toronto (a fund established by an inaugural donation from the Calorie Control Council). He has received food donations to support randomised controlled trials from the Almond Board of California, California Walnut Commission, Peanut Institute, Barilla, Unilever/Upfield, Unico/Primo, Loblaw Companies, Quaker, Kellogg Canada, Danone, Nutrartis, Soylent, and Dairy Farmers of Canada. He has received travel support, speaker fees and/or honoraria from ASN, Danone, Dairy Farmers of Canada, FoodMinds LLC, Nestlé, Abbott, General Mills, Nutrition Communications, International Food Information Council (IFIC), Calorie Control Council, International Sweeteners Association, International Glutamate Technical Committee, Phynova, and Brightseed. He has or has had ad hoc consulting arrangements with Perkins Coie LLP, Tate & Lyle, and Inquis Clinical Research. He is a former member of the European Fruit Juice Association Scientific Expert Panel and former member of the Soy Nutrition Institute (SNI) Scientific Advisory Committee. He is on the Clinical Practice Guidelines Expert Committees of Diabetes Canada, Canadian Cardiovascular Society (CCS), and Obesity Canada/Canadian Association of Bariatric Physicians and Surgeons. He serves or has served as an unpaid member of the Board of Trustees and an unpaid scientific advisor for the Carbohydrates Committee of IAFNS. He is a member of the International Carbohydrate Quality Consortium (ICQC), Executive Board Member of the Diabetes and Nutrition Study Group (DNSG) of the EASD, and Director of the Toronto 3D Knowledge Synthesis and Clinical Trials foundation. His spouse is an employee of AB InBev. AT was funded by the National and Kapodistrian University of Athens. MU was not funded to conduct this work.
Contribution statement
MA, MEJL and AP wrote the introduction. US, JLS, AT and MU wrote the prevention of type 2 diabetes section. CC, MEJL, JIM and ANR wrote the body weight section. A-MA, JIM and ANR wrote the carbohydrate section. ANR, UR, AAR and US wrote the dietary fat section. KH, TK, EP, AP and US wrote the protein section. CWCK, HK, AP, DR, ANR, JS-S and JLS wrote the food-based approaches section. CWCK, HK, DR, JS-S and JLS wrote the dietary patterns section. ANR wrote the environmental sustainability and food processing sections. MA wrote the patient support section. ANR finalised the recommendations. AP convened the Guideline Group. US was head of the DNSG during recommendation development. All authors contributed to editing drafts of the full manuscript, and approved the final version to be published.
Funding
This guideline development process received support from Novo Nordisk Germany, MSD Germany, The Swedish Diabetes Association, Abbott Nutrition, The Finnish Diabetes Association, The Norwegian Diabetes Association, the German Diabetes Association, the National Diabetes Association in Sweden and The Uppsala Diabetes Centre in the form of educational grants. These grants were managed by the not-for-profit organisation DiabCom and only used to facilitate meetings of the Guideline Development Group. The Healthier Lives National Science Challenge of New Zealand funded the design of the graphical abstract. The funders had no role in developing guideline scope, systematic review processes, evidence grading, guideline content, or the release of the guidelines.
Author information
Authors and Affiliations
Consortia
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Guideline Development Group for the Diabetes and Nutrition Study Group (DNSG) of the EASD are listed in alphabetical order in the Appendix. These individuals are the authors of this article.
These guidelines were reviewed for EASD by its Committee on Clinical Affairs.
Supplementary information
ESM
(PDF 159 kb)
Appendix
Appendix
Members of the DNSG Guideline Development Group (authors; in alphabetical order)
Associate Professor Anne-Marie Aas
1. Division of Medicine, Oslo University Hospital, Oslo, Norway
2. Institute of Clinical Medicine, University of Oslo, Oslo, Norway
Associate Professor Mette Axelsen
1. Department of Clinical Nutrition, University of Gothenburg, Gothenburg, Sweden
Dr Chaitong Churuangsuk
1. Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand
Professor Kjeld Hermansen
1. Department of Endocrinology and Internal Medicine, Aarhus University Hospital, Aarhus, Denmark
Dr Cyril W. C. Kendall
1. Department of Nutritional Sciences, University of Toronto, Toronto, ON, Canada
2. Toronto 3D Knowledge Synthesis and Clinical Trials Unit, Clinical Nutrition and Risk Factor Modification Center, St. Michael’s Hospital, Toronto, ON, Canada
3. College of Pharmacy and Nutrition, University of Saskatchewan, Saskatchewan, Canada.
Dr Hana Kahleova
1. Physicians Committee for Responsible Medicine, Washington, DC, USA
2. Institute for Clinical and Experimental Medicine, Diabetes Centre, Praha, Czech Republic
Dr Tauseef Khan
1. Department of Nutritional Sciences, University of Toronto, Toronto, ON, Canada
Professor Michael E. J. Lean
1. School of Medicine, Dentistry and Nursing, University of Glasgow, Glasgow, UK
Professor Sir Jim I. Mann
1. Department of Medicine, University of Otago, Dunedin, New Zealand
2. Edgar Diabetes and Obesity Research Centre, University of Otago, Dunedin, New Zealand
Dr Eva Pedersen
1. School of Pharmacy and Medical Sciences, University of South Australia, Adelaide, SA, Australia
Professor Andreas Pfeiffer
1. Department of Endocrinology Diabetes and Nutrition, Charité Universitätsmedizin Berlin, Berlin, Germany
Associate Professor Dario Rahelić
1. Vuk Vrhovac University Clinic for Diabetes, Endocrinology and Metabolic Diseases, Merkur University Hospital, Zagreb, Croatia
2. School of Medicine, Catholic University of Croatia, Zagreb, Croatia
3. School of Medicine, Josip Juraj Strossmayer University of Osijek, Osijek, Croatia
Dr Andrew N. Reynolds
1. Department of Medicine, University of Otago, Dunedin, New Zealand
2. Edgar Diabetes and Obesity Research Centre, University of Otago, Dunedin, New Zealand
Professor Ulf Risérus
1. Department of Public Health and Caring Sciences, Uppsala University, Uppsala, Sweden
Professor Angela Albarosa Rivellese
1. Department of Clinical Medicine and Surgery, University Federico II of Naples, Naples Italy
Professor Jordi Salas-Salvadó
1. Departament de Bioquímica i Biotecnologia, Institut d'Investigació Sanitària Pere Virgili, Universitat Rovira i Virgili, Reus, Spain
2. CIBER Fisiopatología de la Obesidad y Nutrición (CIBER Obn), Instituto de Salud Carlos III, Madrid, Spain
Professor Ursula Schwab
1. School of Medicine, Institute of Public Health and Clinical Nutrition, University of Eastern Finland, Kuopio, Finland
2. Department of Medicine, Endocrinology and Human Nutrition, Kuopio University Hospital, Kuopio, Finland
Associate Professor John L. Sievenpiper
1. Department of Nutritional Sciences, University of Toronto, Toronto, ON, Canada
2. Department of Medicine, University of Toronto, Toronto, ON, Canada
3. Division of Endocrinology and Metabolism, Department of Medicine, St. Michael’s Hospital, Toronto, ON, Canada
4. Toronto 3D Knowledge Synthesis and Clinical Trials Unit, Clinical Nutrition and Risk Factor Modification Center, St. Michael’s Hospital, Toronto, ON, Canada
5. Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, ON, Canada
Assistant Professor Anastasia Thanopoulou
1. Medical School, National and Kapodistrian University of Athens, Athens, Greece
Professor Emeritus Matti Uusitupa
1. School of Medicine, Institute of Public Health and Clinical Nutrition, University of Eastern Finland, Kuopio, Finland
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
The Diabetes and Nutrition Study Group (DNSG) of the European Association for the Study of Diabetes (EASD). Evidence-based European recommendations for the dietary management of diabetes. Diabetologia 66, 965–985 (2023). https://doi.org/10.1007/s00125-023-05894-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-023-05894-8